NIH Cannot Forget Patients With Chronic Pain
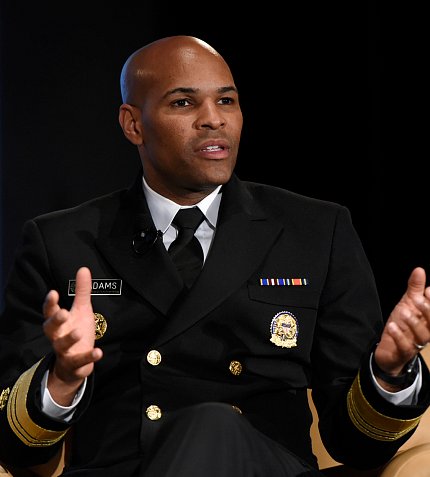
Photo: Andrew Propp
There’s a joint crisis of pain and addiction in America, said NIH director Dr. Francis Collins. On one hand, 25 million Americans report chronic pain daily. On the other hand, an estimated 2 million Americans are addicted to opioid pain relievers.
“If there’s good news, it’s that research has been moving along—particularly research in neuroscience—to revolutionize our understanding of what’s happening in the brain and the peripheral nervous system, both in addiction and in pain,” said Collins during the 2018 NIH Pain Consortium Symposium’s keynote address held recently.
However, scientists must translate those promising basic research findings into non-addictive treatments for pain, he said. Potential alternative treatments might include drugs, devices or even behavioral interventions.
“We need safe and more effective strategies beyond what we have right now, particularly for those individuals for whom opioids are a poor choice,” he said.
In April, NIH announced the launch of the HEAL (Helping to End Addiction Long-term) Initiative, an aggressive, trans-agency effort to speed scientific solutions to stem the national opioid public health crisis. The initiative was made possible by a funding boost from Congress.
“We’re going from basic to behavioral and everything in between. We’re promoting innovative partnerships, including with other government agencies—particularly SAMHSA—and also with advocates and industry,” Collins said.
Ultimately, the initiative will gather more information about what happens when acute pain turns into chronic pain in at-risk patients, identify better targets for pain management, create pre-clinical screening platforms and establish a clinical pain research network.
“We would very much like to have better means of assessing pain, going beyond the unfortunate 1-10 scale, which we all realize is flawed in multiple ways and affects many of the decisions about whether something is working or not,” Collins said.
After the keynote address, U.S. surgeon general Dr. Jerome Adams joined Collins on stage for a fireside chat. As the nation’s doctor, Adams conveys complex scientific information in plain language to the public so people can improve their health and reduce their risk for illness and injury.
Responding to the opioid epidemic is a key priority for Adams. Recently, he wrote a surgeon general’s advisory urging the public to carry the overdose-reversing drug naloxone with them. An overdose can happen anywhere, anytime. Both Adams and Collins carry the drug.
“If we’re going to turn this opioid epidemic around, we need naloxone to be as ubiquitous as CPR,” he said. “Someone could bust down the door right now and say, ‘Someone’s in the bathroom and they’ve overdosed.’”
He believes “stigma is the biggest killer we have out there.” It affects the nation’s ability to respond to the opioid crisis by preventing people from coming forward and admitting they have a problem.
“We’ve got this belief in our country...that pain is just something you’ve got to suck up and have to deal with,” he added.

Photo: Andrew Propp
Lack of access to health care services is another barrier that prevents people from receiving the care they need. When Adams was growing up, he was diagnosed with asthma. To get treatment for their son, his parents drove him to Washington, D.C., a 2-hour drive from his home in rural southern Maryland. If his parents weren’t able to take time off from work, they had to cancel the appointment.
He thinks mental health consults should be a part of routine health care. Instead of asking “What’s wrong?” doctors must ask “What happened?” Many Americans have experienced trauma in their childhood, which leads to increased risk for drinking, smoking, criminal behavior and chronic pain.
Adams would like to work with NIH to write the first surgeon general’s report on trauma and resilience. Collins said the agency would embrace that opportunity.
“We want to minimize the trauma people face, but, at some point, we aren’t going to be able to avoid all of it,” noted Adams. “The question is ‘How do we build resilience?’”
Minorities have been disproportionately undertreated for chronic pain, said Adams. Many patients with sickle cell disease, for instance, don’t receive the treatment they deserve because they’re labeled as drug seekers, he explained.
Adams challenged the audience to think beyond research papers. Scientists’ voices can be just as powerful when they write newspaper opinion pieces or participate in radio show interviews.
“Your voices can be just as powerful and reach more people sometimes in an op-ed in the local paper,” he concluded. “We need to figure out how better to get the message out to the public so there’s a hunger for what you’re working on.”
