Gaming Medical Research
AI Workshop Surveys Landscape, Assesses Big Ideas

Photo: Chia-Chi Charlie Chang
It’s been nearly 160 years since Milton Bradley introduced a “Game of Life” wherein players navigate around a brightly painted board, landing on spaces that dole out good fortune and bad. Although modern editions billed it as a “game of skill and chance,” contemporary Life relied more on the whimsy of a Wheel of Fortune than on personal acumen for success. At the Day of Reckoning you were as likely to wind up a millionaire as a pauper. That’s life, right?
What if players had extraordinary, suprahuman help, though, to foresee dangers, dodge misfortunes and seize advantages? And what if the game ultimately was your real life—or specifically, your health?
That was the fascinating salvo keynote speaker Craig Mundie launched at a recent all-day workshop devoted to “Harnessing Artificial Intelligence and Machine Learning to Advance Biomedical Research.”
We’re seeking prescience about our health, the tech oracle suggested. “How do we structure the problem in such a way that the machine can learn the answer and tell it to us, as opposed to the other way around?” he asked. “This is a big difference between whether you’re just trying to make the machine do what you already know how to do—things it can do more efficiently—or, are you saying, ‘No, the machine can know things I’ll never find out’? That’s a very different way to think.”
Held appropriately in NIH’s on-campus brain center, the Porter Neuroscience Research Center, the meeting gathered thousands of in-person and online attendees—both the AI-experienced and the AI-curious—to explore what NIH director Dr. Francis Collins called “something pretty profound.”
Artificial intelligence, “considered to be the bigger umbrella, can sense, reason, act and adapt,” he said, defining terms at the outset. Machine learning (ML) refers to algorithms “whose performance improves as they are exposed to more data over time, with the learning aspect being the emphasis.”
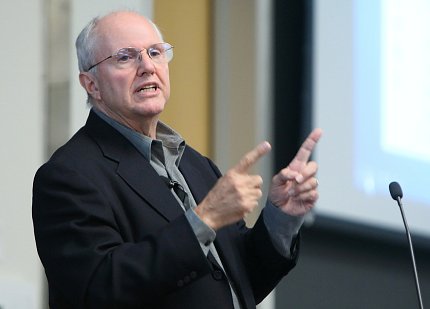
Photo: Chia-Chi Charlie Chang
Collins sought advice on how NIH should engage AI and ML to manage the huge amounts of data the biomedical field is generating and collecting and aim that knowledge toward improving health.
AI, big data, robotics and cloud computing are all included in what some have categorized as “the fourth industrial revolution,” he said, putting the workshop in historical context. “This topic is certainly one that is due for a deep dive by NIH leadership in terms of where we are and where we might need to go.”
The goals of the workshop were to survey the state of AI for biomedical research, dig deeper into specific examples, explore opportunities for NIH to make maximum impact and identify key challenges and obstacles and how can NIH help solve them.
The event also featured numerous innovative ideas presented during two plenary sessions (see sidebar) and discussions afterwards with audience and speakers.
Ultimate Chess Match
Stirring the pot first, though, was former “visionary-in-residence” at Microsoft Mundie with a provocative proposition: AI learns faster and better than humans ever will, so why not give it all of the raw biological data and let the machine learn the pathways and functioning of human biology and use that to predict or find ways to resolve high-dimensional problems such as complex disease?
The longtime tech mega-consultant is known for identifying patterns in information, matching compatible designs and concepts and foreseeing how they could possibly work together to transform whole industries. In the past few years, he’s directed this talent toward the health and biomedical research fields.
Collins invited Mundie to envision NIH’s ideal role regarding the artificial intelligence age; for inspiration, Mundie looked to the computer gaming world. He began by asking a bold question: “Is human biology too complicated for humans to figure out?”
Remarkably in this age of “big data,” he wasn’t endorsing putting more resources into mining gigantic data sets. Mundie’s prescriptions leaned more toward “minimization as opposed to maximization.” So, he posited, we have the human genome and the proteome and maybe that’s as many “omes” as we need to feed into the machines.
“Most of everything we’ve done in data-driven biology and medicine starts with the assumption that we look at a population and try to extract from that population things that we then apply to the individual,” he said. “My prediction is that the future of medicine is all about starting with the individual, and ultimately, as you see enough commonality, you’ll synthesize the population answer—that’s completely upside down from everything the world currently has done.”
Humans, No Monopoly on Knowledge

Photo: Chia-Chi Charlie Chang
Mundie’s “penicillin discovery moment” occurred as he encountered recent reports from the computer gaming community. Professional machine-learning gamers studying how AI could be applied to the ancient game “Go” or to solving Rubik’s Cube were coming to terms with their human frailties—computers were increasingly employing the sheer scale of their AI advantage to beat human experts every time. The machines were synthesizing and learning from the different maneuvers and strategies of millions of iterations of the games in a matter of days—more than any human player could hope to experience in a lifetime.
Then, Mundie observed a chance situation in biology where the learning system compensated for a human error in providing requisite data and got a better answer without it.
“These things learn at a scale that humans cannot do and never will be able to do,” he explained.
Showing an article from the most recent Harvard Business Review, Mundie said, “They like many others are wrestling with the question of ‘What does it mean for mankind when the computer does all of the things that we do?’” They suggest a collaboration between human and machine where the humans provide three key capabilities—training, explaining and sustaining. He questioned whether the first two were really required.
Clue to Health?
Perhaps the biomedical research community—and NIH in particular—should get into the game-design business, Mundie said, sketching an outline of the potential competition.
“Life is just a tournament of multi-player games,” he said. “To win this game, teams have to get the most people to have the longest, highest quality existence. Every game is unique.”
Who are the players? “Mother Nature is a player and she has two tools—randomness and evolution,” Mundie said.
Other contenders are the environment, which includes the physical world as well as political, financial, policy, governance and computing infrastructure factors. Of course, AI and ML—“the bots”—are playing the game too. Their role is to help humans, who include individuals and the people employed in the medical research, health care delivery and wellness and prevention ecosystems.
“This is really an interesting way to think about applying all the different elements of AI to this problem,” Mundie concluded. “This approach discards existing history about biology and medicine and builds an understanding of pathways and interventions up from the individual rather than down from the population. Ultimately, humans will trust—rather than understand—what the machines know and do, just as they do with most of the computerized infrastructure in their lives.”
And how would success be measured? Many in the audience wanted to know.
“What I consider to be winning for me personally, I’d like to live my life where my physical body and my mental capacity stay in sync and in the end they kind of get extinguished together,” Mundie concluded.
The entire workshop is archived at https://videocast.nih.gov/summary.asp?Live=28053&bhcp=1.

