Global Model for Registries
SEER Marks 50 Years of Turning Cancer Data into Discovery

In 1971, the National Cancer Act expanded National Cancer Institute (NCI) authority. As a direct result, the newly established National Cancer Program created a data bank to collect, store, analyze and disseminate data that would support research on prevention, diagnosis and treatment.
This marked the birth of the Surveillance, Epidemiology and End Results (SEER) Program, the main strategy NCI uses to support activities that monitor trends in cancer diagnosis and outcomes. Data collection for SEER began in January 1973 with diagnoses in the U.S. and its territories. Geographic area and demographic coverage have expanded over the past 50 years to represent nearly half the U.S. population today.
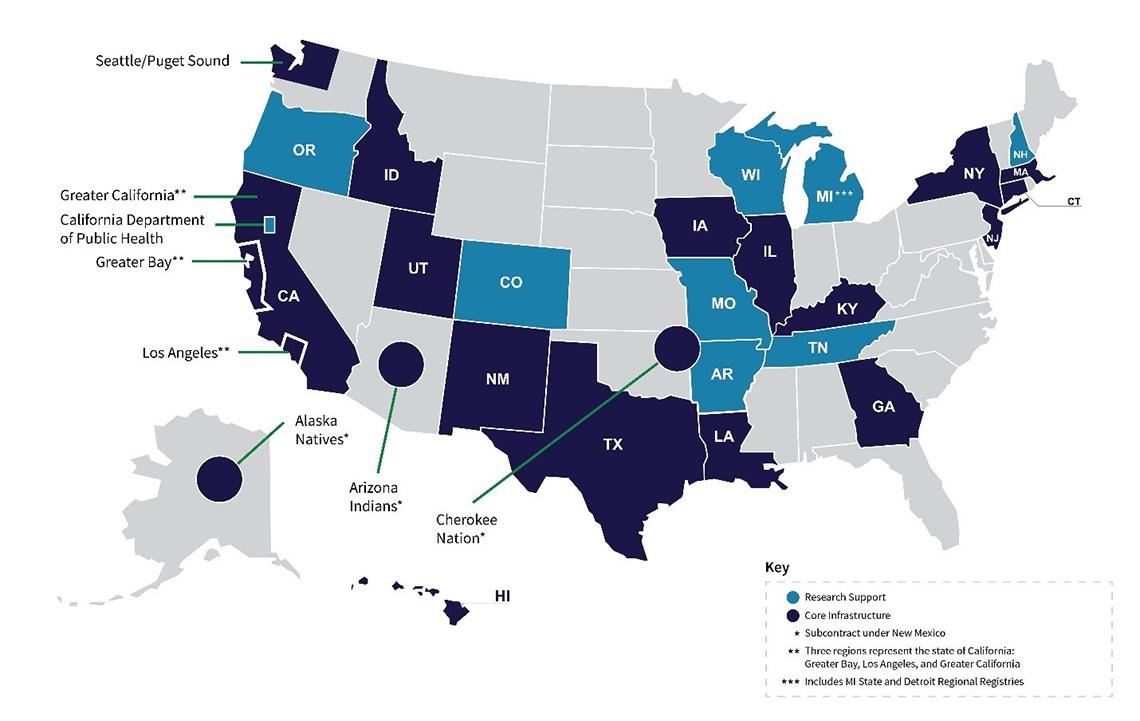
SEER comprises 18 population-based central cancer registries that submit data to NCI and 10 additional registries providing research support.
A cancer registry is an information system that collects, stores and manages data on all people with cancer who reside within the registry catchment area. Registries are the backbone of surveillance, tracking progress of efforts to reduce the cancer burden. The data are used to plan and evaluate cancer prevention and control efforts nationally and at the state level.
De-identified surveillance data also represent a source to support cancer research broadly.
“The [SEER] program serves two really important purposes,” said Dr. Lynne Penberthy, associate director of NCI’s Surveillance Research Program. It “provides population-based estimates on incidence, mortality and survival for cancer in the U.S. and monitors the progress of how we’re improving cancer outcomes over time. The second major purpose is to support cancer research through the controlled access to different de-identified SEER data products.”
SEER is an authoritative source of information on cancer rates and trends nationwide. It also supports multiple types of cancer-related research by providing information on outcomes to evaluate the effectiveness of new treatments among patients outside the clinical trial setting (in the real world) and providing controlled access to various SEER data that support other types of epidemiologic studies.
More than 17,000 publications have included SEER data as part of their primary analysis. Each year more than 4,500 people download the SEER data file.
Throughout its history, SEER has adapted to the changing needs of the cancer research community. For example, cancer surveillance at NCI has expanded to include evaluating patterns and trends in cancer-related risk factors, health behaviors and health services and their effects on trends in cancer incidence, morbidity, mortality and patient survival.
Studies focus on developing and improving methods for cancer-related surveillance research and promoting and facilitating their use among investigators within the extramural community and federal agencies.
Until relatively recently, cancer registrars had to manually enter cancer data into a patient record. Now, patients have electronic health records that require registrars to consolidate information from multiple sources and review it for accuracy.
The SEER Program now works with many health care provider data sources, such as pharmacies and genomic testing laboratories, to enable centralized links to cancer registries, offering comprehensive data with clinical information often not accessible through traditional reporting mechanisms.
And the program has prioritized adjusting to the changing landscape. SEER is moving toward more automation where possible to improve consistency and reduce the delay in cancer reporting.
Given its emphasis on quality control since its inception, longstanding commitment to representing all segments of the population and recent progress in supporting research advances, the SEER Program provides a model for cancer registries around the world.
