Poor Doctor-Patient Communication Often Breeds Poor Care

Photo: Ernie Branson
A doctor’s communication skills might be the difference between patients receiving high-quality care instead of sub-standard care. That’s what NIMHD director Dr. Eliseo Pérez-Stable stressed at the recent CC Grand Rounds: Contemporary Issues in Graduate Medical Education in Lipsett Amphitheater.
“Effective patient-doctor communication leads to better patient satisfaction, better adherence with medications and, ultimately, better health outcomes where adherence to treatment matters,” Pérez-Stable said.
In the late 1990s, he said, then-Oregon Health Science University faculty member Dr. Wendy Levinson studied whether there was a link between the communication skills of doctors and malpractice claims. She discovered that doctors who never had a malpractice claim filed against them asked for patients’ opinions, explained what was going to happen during the appointment, asked for feedback, used more humor and conducted longer visits.
He said the ability to communicate effectively is not a gift, but a skill that can be acquired and improved through hard work. Poor communication between patients and doctors is one factor driving health disparities in the United States.
When a patient first visits, the doctor should ask questions about racial and ethnic background, income level, formal years of education, occupation, parents’ level of education and occupation, residence and preferred language (if not native English speaker). The answers to these questions will give the doctor an idea whether patients are from a population that has higher rates of disease and how best to communicate with them.
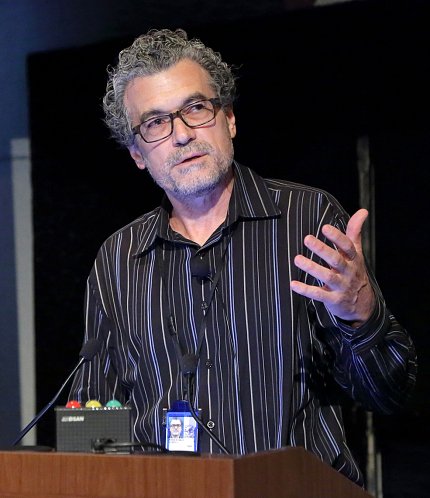
Photo: Ernie Branson
“Most of the time, we don’t obtain anything close to reasonable information in our health care systems on these metrics,” he said. “It’s not just a matter of knowing for research purposes. It’s a matter of knowing for quality of health care.”
Twenty-two percent of Americans read at a 4th grade level, while the average American reads at 8th grade level, Pérez-Stable noted. Those who have difficulty reading have a harder time understanding what a doctor says. They might not be able, for example, to follow dosing instructions on medication labels.
Most patients who can’t read go out of their way to hide that fact, he said. Some, for instance, will ask someone else to read a page because they “forgot their glasses.”
To determine whether patients are functionally literate, Pérez-Stable recommends asking questions such as, “Do you have problems learning about your medical condition because of difficulty understanding written information?” or “How often do you have someone help you read hospital materials?”
When he worked at the University of California, San Francisco, School of Medicine as a general internist, Pérez-Stable asked patients to fill out a form with their medical history before their visit. Some wouldn’t fill out the form completely or even at all.
“Right there is your first sign that there is an issue with literacy,” he said.
When working with patients who have trouble reading, Pérez-Stable advises doctors to think about how they would explain a concept to someone without a medical degree. He also warns against interrupting when patients are talking and suggests avoiding jargon because “people will tune out if they do not understand the medical jargon.”

Photo: Ernie Branson
Communication is more than talking to patients. Doctors should be aware of non-verbal communication such as making eye contact or placing a hand on a patient’s shoulder.
“There are a lot of other traditions, customs and issues around spirituality that matter a lot in dealing with patients from different cultures,” Pérez-Stable said.
In Latin America, he said, a kiss on the cheek is an acceptable greeting in some cases. In other places, however, patients don’t like the intrusion on their personal space and maintain a distance or do not look one in the eye.
In patient-centered care, the gold standard is shared decision-making. He cautioned, however, that it can “be taken to the extreme.” As an example, he said, most people have difficulty interpreting the risk of getting a disease. Doctors cannot assume patients make the best decision.
If, for instance, a person has a 10 percent chance of having a heart attack in the next 10 years, clinical guidelines say patients should take statins to lower their cholesterol. However, some people will think they have a 90 percent chance of not having a heart attack, so they don’t see the rationale for taking statins. In clinical situations like this, a strong clinician recommendation may be a better approach than a “shared-decision” model of care.
Speaking the same language as a patient is also important because doctors make fewer mistakes when they do. In the event it isn’t possible for a doctor to speak the same language as a patient, professional interpreter services delivered in person, through video conferencing or telephone are strongly recommended alternatives.
Some hospitals, including where Pérez-Stable used to work in California, offer small financial compensation to physicians who know a second language well enough to use with patients. “That’s not what motivates people, but at least it’s some recognition,” he noted.
Pérez-Stable concluded by reminding doctors to let patients speak without interruption and to be concrete and specific when making a recommendation to a patient and avoid technical language.
