Mighty Microfluidics
Pompano Builds New Lymph Node Models

You may be painfully aware of the lymph nodes in your neck when you are sick with a cold. But did you know that they are just some of the roughly 600 lymph nodes found throughout the human body? Lymph nodes house immune cells and are important for fighting off infection.
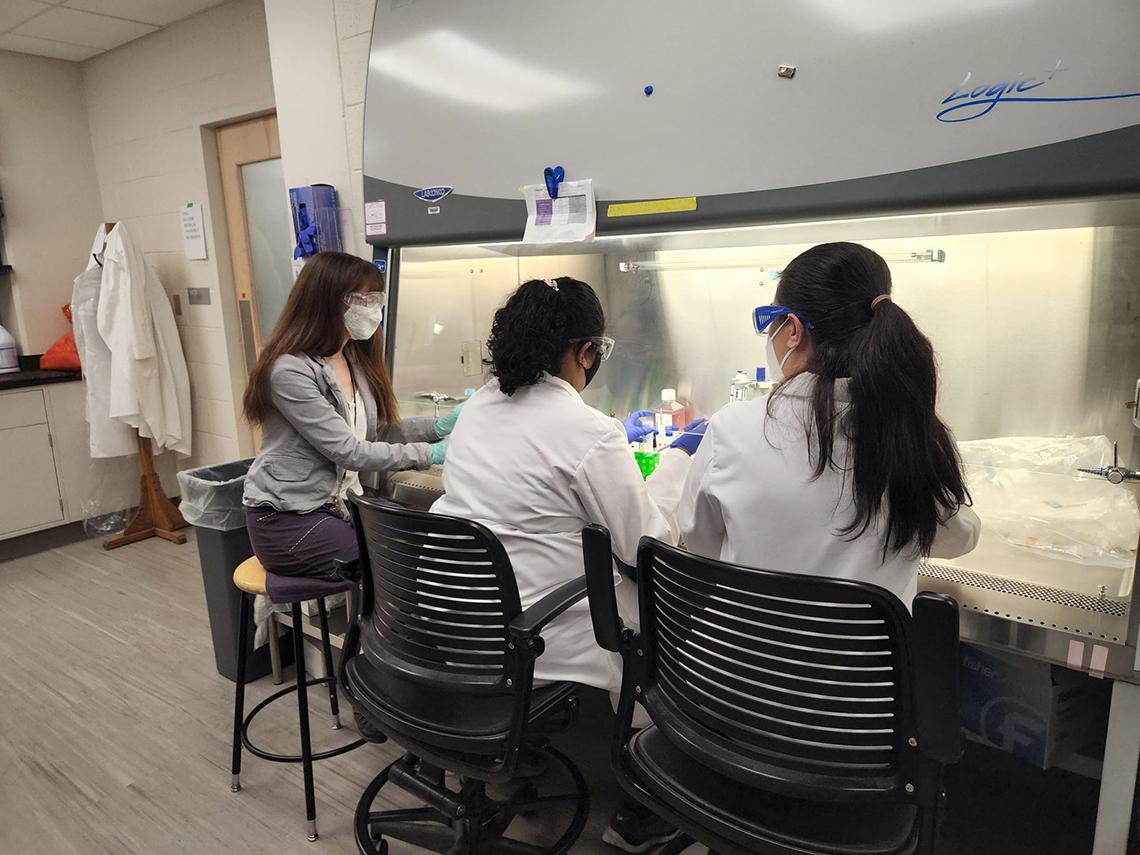
But researchers have limited options for studying lymph nodes in the lab. Dr. Rebecca Pompano of the University of Virginia is working to change that. She recently presented on her research in a lecture, “Modeling Vaccine Responses and Tumor Immunity Using Microfluidics,” hosted by the Biomedical Engineering Scientific Interest Group.
Historically, study of lymph nodes has been “kind of a niche field in immunology,” she said, and model systems are “lacking.” Her lab is developing groundbreaking technology to combine live lymph node tissue with microfluidic devices.
To some, Pompano might seem an unlikely scientist to pursue lymph node research. She received her doctorate in chemistry and only began working in immunoengineering during a postdoctoral fellowship. She has continued to conduct research in that area and her UVA lab works at the intersection of chemistry, engineering and basic science.
Prior to Pompano’s research, most labs either used cells from crushed lymph node tissue or studied lymph nodes in animal models. When she started her lab in 2014, Pompano was inspired by advances in microfluidics and wanted to incorporate it into her research. Microfluidic devices are tissue chips (3D-printed or made from silicone rubber) that move small amounts of fluid through the tissue via tiny channels.
From the Ground Up
Before they could even begin to use microfluidic devices, Pompano first had to figure out a method for obtaining tissue slices. Existing culture systems (using animal models, or removing the organs and crushing them up to measure the cellular secretions) were unsuitable.
Neuroscientists are familiar with brain slicing—a device is used to slice the organ into thin cross-sections and then the slices are viewed under a microscope. Pompano’s lab adapted this technique for lymph nodes, using a vibratome— “essentially a $20,000 bread slicer,” according to Pompano—to cut the roughly 2-millimeter-long mouse lymph nodes. Then, the slices can be seen with a microscope or transferred to a microfluidic device. The segments are particularly useful for preserving the organs’ spatial structure while keeping them alive.
Pompano’s microfluidic devices were also established out of the need to develop a new method for local drug delivery to a piece of tissue.
Tissue chip technology has been around for several decades, but the Pompano lab adapted it for their own use in several ways.
First, they developed a system in which they could “co-culture” two pieces of tissue (such as a lymph node slice and a tumor slice). They ran fluids through micro-channels in the chip to mimic the flow of interstitial fluids and carry secreted factors between the two tissue samples. This system was crucial for Pompano’s research, because, as she noted, “no organ is an island…particularly the lymph nodes.”
The team ran into several problems: the initial chips were made of silicone rubber and were very time-consuming and difficult to build. Also, the set-up required to pump fluid was complicated.
Pompano quickly realized that collaborators might not want to work with such a complex configuration in their own labs.
One of her Ph.D. students, Sophie Cook, redesigned the chips, using a 3D printer instead of silicone and employing technology from a common lab item—a magnetic stir plate—to move the fluid instead of bulky pumps. The resulting chip was far easier and quicker to construct—assembling in a matter of hours rather than days.
Asking New Questions

With these new research techniques, Pompano is able to investigate exciting new research questions.
She vaccinated mice in vivo with an egg-derived antigen called ovalbumin (abbreviated OVA), obtained lymph nodes four days later and sliced them. She treated these slices (plus unvaccinated control slices) with another OVA antigen that would fluoresce green if taken up by a cell.
She observed that the fluorescent antigen was picked up in both conditions, demonstrating that lymph node slices were capable of processing antigens even after vaccination.
The lymph node co-culture technology has potential for areas like tumor immunity research. Pompano and her colleagues co-cultured lymph node slices with either tumor slices or healthy fat tissue (from the same animal). The researchers then checked the lymph nodes’ immune response by measuring T cell activation and one specific cytokine secreted by the T cells.
If the lymph node slice was co-cultured with healthy tissue, then the lymph node secreted plenty of cytokines, which is the normal response.
Interestingly, when tumor tissue was used instead of healthy tissue, Pompano saw a “small but significant reduction” in the amount of cytokines secreted. The immune response was suppressed, just like what happens in the body. Researchers think that suppression might contribute to why the immune system doesn’t attack cancer cells, so it was exciting to see it replicated on the chip.
Ex Vivo Vaccination?
Another futuristic-sounding application is vaccination—of the microfluidic chips. This is still in progress, but preliminary research has yielded promising results.
In a typical vaccination, the antigen has to travel into the lymphatic system in order to produce an immune response. To mimic this process, Pompano pipetted a labeled antigen (representing a vaccine) into one tissue well and then watched to see if it would travel into the lymph node slice downstream from the injection slice. Four hours later, she saw the antigen had entered the lymph node slice.
Pompano continues to test this response in new studies.
Up Next: Human Immunity

Pompano and her group are also starting to study human immunity, using “waste” from common medical procedures such as tonsils and white blood cells (from platelet donations). Her future goals include using these human tissue sources in co-culture with other organs to study vaccines and infection, autoimmunity and tumor and brain immunity.
“There’s [almost] too much to do,” she laughed. “It’s a challenge and a joy.”
To view the archived lecture, visit https://videocast.nih.gov/watch=48967.
