Symbiotic or Sinister?
Sears Reveals Microbiome’s Role in Colon Cancer

How does colon cancer start?
According to research from microbial detective and Johns Hopkins University professor of medicine Dr. Cynthia Sears, microorganisms in the human gut microbiome may contribute to the development of cancer (oncogenesis). She revealed her findings in the hybrid lecture “Sleuthing the Microbiome Reveals Undercover Agents of Oncogenesis,” which was also the 26th iteration of the annual Astute Clinician Lecture Series. The series honors U.S. scientists who have observed unusual clinical occurrences and, by investigating them, have opened important new avenues of research.
Sears began her career as an infectious disease specialist studying gut infections, and now focuses on how microbiota and specific bacterial pathogens contribute to colon carcinogenesis. In her lecture, she sought to “give a framework for how we consider microbes in the pathogenesis of human colon cancer.”
The gut microbiome consists of microorganisms—such as bacteria, viruses, fungi and archaea—that often have a mutually beneficial relationship with their host. However, Sears has discovered, changes in these microbes can alter the cells lining the gut (epithelial cells) in ways that make them more likely to become cancerous.
What causes changes to gut microbes? There are many factors, but one specific culprit Sears identified is antibiotic usage. Antibiotics are useful tools for treating infectious diseases, but, she said, doctors “must consider how antibiotic exposure over the lifetime [can be] an ever-evolving disease modifier, potentially with a high impact on disease development.”
Using data from the United Kingdom Clinical Practice Research Datalink, Sears and collaborators matched colon cancer patients with healthy controls of similar backgrounds. The researchers found an increased association between the incidence of colon cancer and the patients’ use of oral antibiotics more than 10 years prior to receiving a colon cancer diagnosis. Other studies have validated these findings. For Sears, these results highlight how antibiotic-mediated shifts in the microbiome may contribute to the development of chronic disease.
How do disruptions to the gut microbe population lead to cancer?

Photo: Ben Schonewille/Shuttershock
Sears discussed Bacteroides fragilis, a common bacterium in the colon that is typically harmless—unless it is a certain strain known as ETBF, or enterotoxigenic B. fragilis. ETBF is pro-inflammatory and tumorigenic by way of the B. fragilis toxin (BFT) gene it possesses. There is also a non-toxic B. fragilis (NTBF) that does not have BFT. Not everyone with ETBF in their colon will have symptoms—it has been isolated in both healthy people and those with gastrointestinal disruptions such as diarrhea—but it is hypothesized that factors such as stress and antibiotic use may disrupt the gut microbiome and make ETBF more likely to induce inflammation.
Using a genetic mouse model permissive to colon tumor formation, Sears has found that a single oral introduction of ETBF causes rapid tumor formation—she could see evidence of microscopic tumors (microadenomas) one week post-inoculation. However, she has also found that if she deletes the BFT gene, “we obliterate all that tumorigenesis.”
How does ETBF promote tumorigenesis on a cellular level?
The colon is lined with epithelial cells that are bound together with a protein called E-cadherin. BFT binds to the epithelial cells and splits E-cadherin. The now-separated epithelial cells undergo marked changes resulting in, for example, DNA damage, which makes cells more likely to become cancerous in the future.
Sears has a “hit list” of 11 bacterial species (including B. fragilis) that are “credible contributors” to colon cancer pathogenesis. But microbes can also work together as a grouping of microbial cells bound together by a matrix on the surface of the gut epithelium, known as a biofilm. Sears found that, in non-hereditary colon cancer, biofilms were often present on the tumor surface, within the tumor and also on the epithelium around the tumor.
Through her research, she has learned that biofilms can be pro-carcinogenic. Epithelial cells in the gut are coated with a double layer of mucus, but biofilms can sometimes penetrate the mucus and damage the integrity of the epithelial cells by cleaving E-cadherin, likely through a similar mechanism to B. fragilis. Interestingly, tumors on the right side of the colon are more likely to be biofilm-positive.
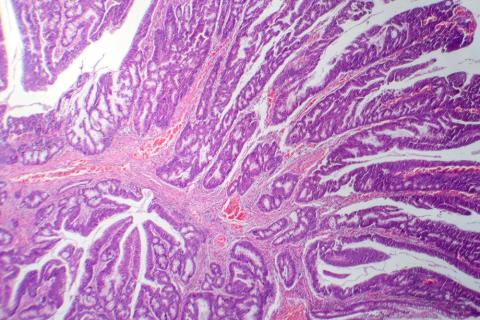
Photo: Kateryna Kon / Shutterstock
The notorious bacterium Clostridioides difficile (C. diff) may have something to do with that. C. diff infection can occur in people whose gut microbiome has been disrupted (typically as a side effect of antibiotic treatment), causing severe colon inflammation and damage.
Two toxins in C. diff (abbreviated TxA and TxB) are most strongly associated with disease in humans, and Sears has learned that TxB in particular “promotes biofilm invasion deep into colonic crypt cells,” where stem cells that replenish the gut epithelium over a person’s lifetime are produced. If the stem cells’ genetic material are damaged, then they may develop mutations that could lead to cancer.
Sears tested this in a mouse model. One group of mice were infected with a TxB-positive strain of C. diff, while the other were infected with the same strain of C. diff, but with the TxB toxin removed. The latter group of mice still had the C. diff in their colons but did not develop tumors; in contrast, Sears said, “the [TxB]-positive community induced tumors…which [appear] to be driven by [the] singular virulence gene” that produces TxB.
Do the other species in biofilms also play a role in tumorigenesis? Sears and her collaborators are now investigating this.
Early studies indicate that other bacterial species may help C. diff be “a chronic colonizer of the human gut,” Sears said, but there is much more work to be done on the mechanisms of how this occurs.
She also wants to hone in on C. diff’s linkage to colon cancer. It’s a “totally new topic for the field,” she observed, and one Sears is excited to explore more.
To watch the lecture, visit: https://videocast.nih.gov/watch=51118.
