Window of Opportunity
Gaucher Disease Provides New Insight into Parkinson’s
Geneticist Dr. Ellen Sidransky likened her research to a saying by Chinese philosopher Confucius.
“I live in a very small house, but my windows look out on a very large world.”

The small house in question is Gaucher disease (GD), a rare condition Sidransky’s lab has studied over the past 20 years. Sidransky is a senior investigator in the Medical Genetics Branch and chief of the National Human Genome Research Institute’s (NHGRI) molecular neurogenetics section. She recently spoke as part of the NIH Neuroscience Seminar series.
GD is a recessively inherited lysosomal storage disease affecting an enzyme called glucocerebrosidase (GCase). This malfunction is encoded by a single gene called GBA1.
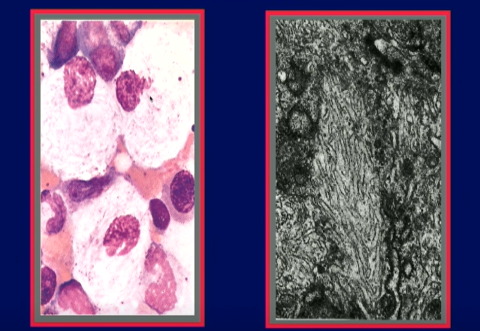
Lysosomes are organelles within cells that use enzymes to break down biological waste. The enzyme GCase digests a lipid called glucocerebroside. Lysosomes are particularly abundant in a type of white blood cell called macrophages and, when GCase cannot break down its target, the macrophage progressively fills with the undigested glucocerebroside lipids. Patients experience a toxic accumulation of glucocerebroside in the liver, spleen and blood marrow, causing a wide array of signs and symptoms.
Sidransky’s past work led to the discovery that a rare subset of patients with GD, as well as some asymptomatic carriers of variants in the GBA1 gene, develop Parkinson’s disease (PD).
But how does this knowledge help researchers better understand PD? Sidransky became interested in the connection between the two diseases in the mid-90s when one of her patients with GD developed features of PD. Could glucocerebrosidase deficiency play a role in the development of PD, Sidransky wondered?
The lab’s next step was a genotyping study comparing individuals with PD to healthy controls. Remarkably, individuals with PD were over five times more likely to carry a variant in in the GBA1 gene. A subsequent study of patients with dementia with Lewy bodies (DLB) showed a similar phenomenon.
“Variants in the Gaucher gene are now the most commonly known genetic risk factor for Parkinson’s disease and Lewy body disorders,” said Sidransky.
What causes this association? There are two prevailing theories—involving a gain- or loss-of-function role for GCase—but Sidransky does not believe there is one single cause.
“The story has to be a lot more complicated,” she said. “We clearly needed new tools and strategies.”
The lab’s first step was to establish cellular models using human cell lines generated from patients with GD and PD; they selected dopamine-producing (dopaminergic) neurons via induced pluripotent stem cells (IPSC) as their model of choice. They also needed to develop a method to measure GCase activity inside of lysosomes. They have produced three so far: a GCase antibody that only shows up in the lysosome, a lysosomal probe and a small tag made of amino acids.
Sidransky’s lab has a clinical study of patients with GD and Gaucher carriers with and without PD at the NIH Clinical Center.
One longitudinal study is looking to determine if they can find early clinical and imaging features predictive of parkinsonism in patients with GBA1 mutations. Studying a group of patients with both GD and PD, they found that some, although not all, have early motor and non-motor findings, and may have earlier and more significant cognitive impairment.
Another longitudinal study followed patients considered at-risk for PD, who either had GD or were carriers. Most also had a family history of PD but, interestingly, only one of the 125 at-risk participants evaluated developed PD.
Sidransky would like to see further longitudinal studies in this area with larger cohorts. Based on her current findings, she said, “it seems like most GD patients are not on a Parkinson’s trajectory,” which is certainly good news for her patients.
“How do we explain this very low penetrance?” Studies thus far indicate that GBA1 mutations are a risk factor for PD, but it seems that there are other factors at play that have yet to be discovered. Sidransky believes genomic approaches will be a valuable addition to clinical evaluations in elucidating these risk factors.
One promising area of study is sibling pairs, in which one sibling has GD alone and the other has both GD and PD. Genomic studies might reveal alleles that are protective against or serve as risk factors for PD. Sidransky’s lab has a small ongoing study with 10 sibling pairs.
The connection between GD and PD may be helpful for advancing treatments for both conditions. Current treatments for GD—enzyme replacement therapy and substrate reduction therapy—do not cross the blood-brain barrier. Sidransky’s lab is looking for ways to help therapeutics cross into the brain.
One contender is a GCase “chaperone,” a small molecule that helps GCase fold properly and reach a lysosome, restoring the full biologic process. This method may ultimately be cheaper and more efficient than the current GD therapeutics and may prove useful in PD treatment as well. Working with collaborators from the National Center for Translational Sciences, they have identified some promising candidates to pursue.
“This emphasis on new tools has provided us with new opportunities” for treating GD and PD, Sidransky reflected. Additionally, she said, studying a rare disorder can have wide-reaching benefits.
“Studies on a rare disorder can come together in many different ways and provide a window into complex disorders that can ultimately be translated into new therapies for both disorders,” she concluded.
A recording of the lecture can be found at https://videocast.nih.gov/watch=55322.
