56 Years Later
NIAID Scientists Find Gene Behind Colleague’s Eponymous Syndrome

“There is real value in experimental odysseys,” says Dr. Thomas Waldmann of the National Cancer Institute.
The NIH distinguished investigator celebrated a new leg of one such journey this summer. In June, colleague Dr. Michael Lenardo, an investigator at the National Institute of Allergy and Infectious Diseases, published his finding of a genetic cause and potential treatment for a subset of the gastrointestinal disease Waldmann had discovered in 1961. Lenardo, who Waldmann recruited to NIH more than two decades ago, will join Waldmann to give a Clinical Center Grand Rounds lecture on their discoveries in Masur Auditorium, Bldg. 10 on Oct. 15.
In 1956, Waldmann came to NIH from Harvard Medical School and Massachusetts General Hospital, where he had received his first research grant totaling $50. At NIH, he began research on how the body metabolizes proteins in the blood, including protective immune proteins called immunoglobulins, or antibodies. Not long after joining NCI, a personnel change put the young researcher in charge of ongoing projects at the institute’s Metabolism Branch. “So I, with a total research experience of a $50 grant, was de facto a tenured investigator,” remembered Waldmann, who now serves as chief of the Lymphoid Malignancies Branch at NCI’s Center for Cancer Research.
Taking advantage of what was then the relatively new Clinical Center, Waldmann’s group began to work with patients who had unusually low levels of immunoglobulin. At the time, he recalls, most physicians believed such patients were simply not making enough immunoglobulin. While this was true for many disorders, he identified a group of patients among those with low immunoglobulin whose symptoms appeared to have a different cause.
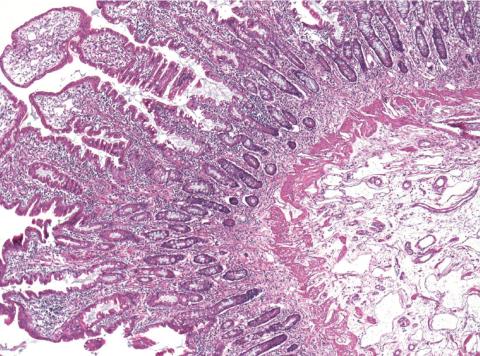
By radiolabeling immunoglobulin in the blood, the lab discovered that some patients were losing these essential antibodies through abnormal lymphatic channels in their digestive tract. As a result, the patients developed symptoms in early childhood, were prone to infections, experienced severe intestinal distress and were not likely to survive into adulthood.
After initially describing this condition in Gastroenterology in 1961, Waldmann and his colleagues published a comprehensive report on the condition in the Journal of Clinical Investigation in 1967. The team dubbed the disease primary intestinal lymphangiectasia, while the National Organization of Rare Disorders called it Waldmann’s disease.
More than four decades later, Lenardo, chief of the molecular development of the immune system section in NIAID’s Laboratory of Immunology, encountered a similar set of children through his collaborators in Turkey. Like Waldmann’s patients, they had low levels of protective antibodies, intestinal distress and other symptoms of primary intestinal lymphangiectasia, such as swelling of the extremities and a predisposition to life-threatening blood clots.
Recognizing the opportunity to further illuminate the rare condition, Lenardo and his colleagues analyzed the genes from 11 children with this subset of primary intestinal lymphangiectasia and their families. Each child had two copies of a defective gene called CD55 that prevented the production of a cell surface protein also called CD55. This protein helps regulate the immune system by blocking the activity of a group of proteins called complement.
Complement can help fight infections by punching holes in the cell membranes of bacteria and other infectious agents, but can also—if left unchecked—damage the body’s tissues. This unchecked complement activity, Lenardo explained, may account for the symptoms experienced by patients suffering an ailment they dubbed CHAPLE disease, or CD55 deficiency with hyperactivation of complement, angiopathic thrombosis and protein-losing enteropathy.
This investigation could not have been imagined in the 1960s, but is now possible due to advances in genetics research. “When new techniques, new approaches, new people look back at the same subset of patients,” said Waldmann, “new discoveries are made.”
Remarkably, Lenardo and his colleagues not only defined a genetic cause for CHAPLE disease but also identified a potential treatment for the disorder, which previously had no specific therapy.
As soon as they understood the mechanism behind the disease, Lenardo’s team got to work testing drugs already approved by the Food and Drug Administration for other diseases to see if they blocked complement activity in samples of their patients’ immune cells. They found that eculizumab, a therapeutic antibody approved to treat another rare condition called paroxysmal nocturnal hemoglobinuria, successfully decreased complement production in the cells.
“People with CHAPLE disease lack CD55 protein and, with it, the ability to control complement activity,” said Lenardo in a release following publication of his findings in the New England Journal of Medicine. “The question is whether treating people with a substitute for CD55’s activity can help slow or reverse the symptoms of this disease.”
Physicians from Lenardo’s group and other teams around the world are now studying eculizumab in people with CHAPLE disease with the hope that the therapeutic could become the first effective treatment for the disorder—a profound discovery for a disorder first described decades earlier in the very same research hospital.
