Kaelin Advocates Robust Approach to Cancer Research

Photo: Chia-Chi Charlie Chang
Dr. William Kaelin, Jr. has a message for young investigators entering medical research: “The most dangerous result in science is the one you were hoping for, because you declare victory and get lazy.”
For example, some investigators rush to link their favorite gene to a prognosis so as to proclaim clinical relevance, said Kaelin, a clinician who is a Harvard Medical School professor and Howard Hughes Medical Institute investigator. He tells his students to do better: think logically, speak clearly with words that have precise meanings and don’t assume correlation together with plausibility proves causation.
“You have to be careful with inferring causality,” said Kaelin, speaking at a recent Wednesday Afternoon Lecture in Masur Auditorium. “Showing that a protein is associated with a bad prognosis in a given cancer is not sufficient to claim it is a good cancer target.”
A focus of Kaelin’s research is hypoxia, or oxygen deficiency. Within a tumor, hypoxia is usually associated with a bad prognosis, he said. Many therefore argue hypoxia causes aggressive tumor growth. But Kaelin cautioned that aggressive tumors can become hypoxic when they outgrow their blood supply. “So one can’t always be sure whether hypoxia is the cause or the result of aggressive tumor growth.”
A central thrust of Kaelin’s talk was robustness. “If a result is true, but only true in your favorite cell line, and it had to be Friday, and the Red Sox had to have won the night before, the result might be true but not robust, and we need [results] that are highly robust,” Kaelin said, illustrating a persistent problem in medicine that he’s written and spoken about extensively—reproducibility.
Many experiments have outcomes that hold true only under narrow conditions, Kaelin warned, making it difficult for other researchers to replicate those results. Experiments that are robust—able to withstand a variety of conditions—are more likely to have practical implications, he said, such as in human clinical trials.
Kaelin’s lab studies tumor-suppressor genes. When these genes mutate, they remove brakes that help prevent cancer. His experiments on certain proteins encoded by these genes hold the potential for new drugs against cancer and other diseases. Yet in recent years, Kaelin noted, a staggering number of papers nominating new cancer drug targets contain irreproducible results, which impedes the development of new drugs.
When it comes to validating preclinical cancer targets, Kaelin said, corroborating lines of evidence are a scientist’s best friend. As a postdoc in the 1980s, he would write a paper using multiple arguments to prove a concept; today, he said, papers often cite a variety of concepts, each proven only one way.
In today’s funding environment, many investigators feel compelled to have their papers culminate in experiments that feel translational, even if rooted in basic science observations that in years past would have been more fully developed and explored, he said. “And honestly describing unexpected findings can be a death knell for publication.”
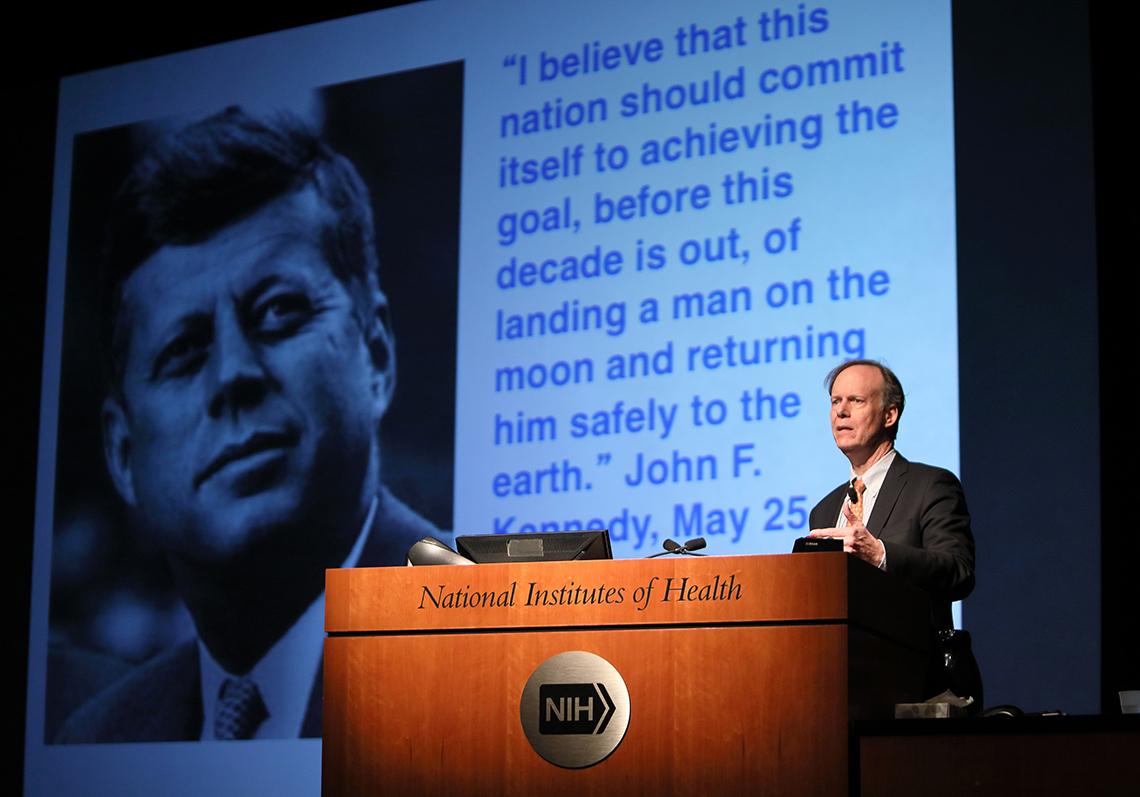
Photo: Chia-Chi Charlie Chang
Kaelin recalled submitting a paper in which he treated eight different renal carcinoma cell lines with a new anticancer drug. The editor initially wanted to reject the paper because several cell lines didn’t react to the inhibitor as Kaelin expected and he couldn’t yet explain why. Demanding that papers have no unanswered questions can delay progress and contribute to the robustness problem, he argues.
“Many people would have cherry-picked the data from the responding cell line models and buried the data from the non-responder models,” said Kaelin. “Then someone comes along and doesn’t see the expected result when they study one of the non-responder models.”
One scientist’s unexplained results or unexpected findings can lead to another researcher’s new discovery. Subsequently, the kidney cancer drug in question went into trial with some encouraging results. But just as predicted by the laboratory experiments, some patients seemed to respond and others did not. And heterogeneous responses are the rule rather than the exception in the clinic.
For example, Kaelin described his work on leukemias caused by IDH mutations. IDH mutations cause the production of 2-HG, an oncometabolite that causes certain cancer cells to proliferate. His group showed that blocking 2-HG production inhibited leukemic cells in the laboratory. A drug that blocked 2-HG production indeed worked remarkably well in clinical trials, but only for about 30 percent of patients.
Kaelin also implored his fellow scientists to work harder to show that the chemical and genetic tools they use in the laboratory are having their cellular effects by inhibiting their intended targets rather than by unintended actions on unsuspected targets. A drug may seem to be the next miracle in the lab—until further study. “The rosiest interpretation is everything is on-target and the model is correct,” said Kaelin. “A good scientist also considers the least interesting interpretation to their data.”

Photo: Chia-Chi Charlie Chang
Even with a good drug, responses to targeted agents are often short-lived, said Kaelin, so there’s not much chance of a cure with a single agent. That’s why combining drugs remains so critical. “The classical way to avoid resistance is to combine drugs that have distinct mechanisms of action, are not cross-resistant with one another and have toxicities that don’t overlap in a prohibitive way.”
Sometimes, a drug all but discarded can lead to new paths in drug development. Thalidomide—given to pregnant women in the 1950s until it was found to cause severe birth defects—and related drugs such as lenalidomide have turned out to be useful drugs for certain malignancies, notably multiple myeloma. Kaelin and Ben Ebert at Harvard, working in parallel, showed that thalidomide-like drugs bind to a protein called cereblon and reprogram it to destroy a protein needed by multiple myeloma cells.
Kaelin also commented on the role academic investigators play in the biomedical ecosystem. He noted that scientists learn the rules of a system and engineers apply that knowledge to do useful things. “Historically,” said Kaelin,”the secret sauce in biomedical research in this country has been the symbiotic relationship…between pharma companies on the engineering side and investigators doing the science.”
Kaelin’s motivation for sharing his observations goes beyond professional interest. It comes as a personal plea in memory of his late wife, Carolyn, a renowned breast cancer surgeon who lost her 4-year battle with glioblastoma in 2015.
“One of many frustrations in treating my wife was that everything I had available to treat her was really based on science that was done 10 or 20 years ago,” said Kaelin.
In the coming years, cancer patients will rely on the science being done now. “The first questions should be: Is this [research] true and robust? Is someone likely going to be able to build on this?”
Kaelin lauded NCI’s Cancer Moonshot but said it was the “right mission, wrong metaphor.” Putting a man on the moon was an engineering feat limited by resources; curing cancer is a scientific effort limited by lack of knowledge; much remains unknown, including the time lines for cures.
“If you’re going to put a man on the moon, you want everyone going in the same direction,” he said. “But people who tell you how truly transformative science gets done would tell you—especially in the early days—you’d be better off having 10 people going in different directions, looking under rocks, and hoping 1 or 2 of them actually discover something.”
Kaelin concluded with a message: “My wife never gave up. To the young people—please don’t give up.”
