West Offers Ideas for Managing Physician Burnout

Photo: Marleen Van Den Neste
Most of us loosely use the word burnout from time to time, but in a lecture delivered at Clinical Center Grand Rounds recently by Dr. Colin West of the Mayo Clinic, the specific definition of burnout was clarified as a syndrome with three main domains: depersonalization, emotional exhaustion and a sense of low personal accomplishment. All lead to decreased effectiveness at work.
“This is a workplace phenomenon,” West said. Burnout is defined as emotional weariness—a feeling of nothing left to give to your patients—and depersonalization—a sense of becoming callous toward the experiences of others. About 40,000 medical students, 60,000 residents and fellows and nearly half a million physicians experience burnout symptoms at any given time in the United States.
Medical students begin their careers with lower burnout than their age-matched peers, West said. There is something wrong with a system that leads these individuals to experience higher rates of depressive and burnout symptoms than their age-matched peers by the second or third year of their medical education, he added. Physical, mental and emotional quality of life domains also flip from the first to the third year.
In a 2008 study of internal medicine students, the burnout rate was 51 percent, and the depersonalization rate was nearly a third of the number of people studied. “This is not what we are looking for from a professional ideal standpoint, for ourselves or for our future colleagues, as the next generation of people taking care of all of our patients and taking care of us,” West observed.
Three surveys on practicing physicians done in partnership with the American Medical Association show that although the overall rate of burnout decreased during the period 2014-2017, a quarter to a third of individuals would meet the criteria for depression if they went through a medical assessment. Also, during this time a substantial number of physicians with burnout were likely to have retired from practice, reducing the overall burnout rate among respondents.
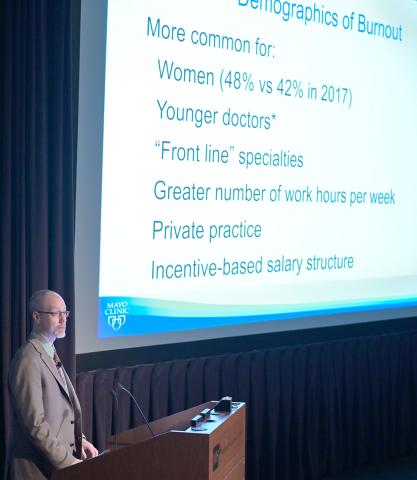
Photo: Marleen Van Den Neste
“Physicians who are burned out are more likely to reduce their [hours] and are more likely to retire early,” West said. This “career survival bias” might be responsible for underrepresentation of late-career physicians with burnout in well-being surveys, leading to overall falsely positive estimates of burnout rates.
Medical professionals experience the highest overall burnout rate compared to other professions, including scientists. Higher burnout rate is correlated with frontline specialties such as emergency medicine and primary care and with tours of duty exceeding 50 hours per week. “Burnout at work results when demands of the job chronically outstrip the resources that are available to support that job,” West said.
Why care about burnout when physicians are better compensated than most other professionals? A mix of negative outcomes—such as diminished patient satisfaction, reduced hours, switching jobs, early retirement, depression, suicidal ideation and public safety issues such as increased accidents and near-miss rates for internal medicine residents—has been conservatively estimated to cost the health care economy roughly $4.6 billion a year, according to a study done in partnership with Harvard Business School. “That $4.6 billion doesn’t appear in any economic analysis of our health care system at this point; I cast this as a public health crisis,” West stated.

Photo: Marleen Van Den Neste
Some of the ways to address physician burnout are increasing control, flexibility and autonomy on a workday; promoting respect for work-life balance and opportunity to focus on job areas that one is more efficient at; improving organizational culture, that is, alignment of stated leadership values with those of the employees and leadership actions; and providing social support groups in the work environment. “Targeting these drivers builds well-being by strengthening the hub of meaning, values and purpose,” West said.
Some individual strategies to combat burnout are identification of personal values, nurturing personal activities, not putting one’s life on hold until a target is achieved and internal reflection about one’s well-being.
System-level policies to promote physician well-being include actively supporting individual focused interventions such as self-care workshops and small group/community building around well-being and enacting structural interventions, such as shorter attending rotations.
Studies by West’s group at Mayo Clinic have shown that a small amount of protected time during the workday resulted in increased meaning from work and reductions in burnout. He also stressed that there should be a dialogue between management and employees on what interventions work best for the workforce.
