Mental Health a Concern
JHU’s Everly Prescribes ‘Psychological First Aid’ During Pandemic

Founding father Thomas Paine certainly could have been writing about 2020, when he said in The American Crisis, “These are the times that try men’s souls.” (Of course, being enlightened, he would’ve included women’s souls too, and noted that the crisis is global.)
Caveats aside, most authorities on mental health agree that the enormous psychological toll of the Covid-19 pandemic—and the measures we’ve all had to take to limit its spread—must be acknowledged and addressed before we can get back to any kind of normal.
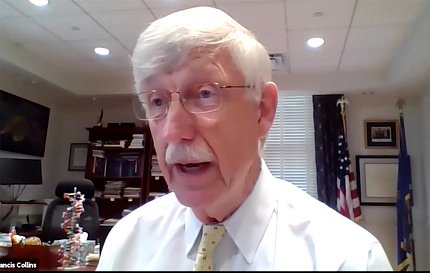
For insights and coping strategies on the problem, NIH director Dr. Francis Collins called on world-renowned expert on psychological impacts of disaster Dr. George Everly, psychologist and professor at Johns Hopkins University’s Bloomberg School of Public Health. He gave a virtual presentation, “Psychological Aspects of Pandemic and Human Resilience,” aimed specifically at the NIH workforce.
Acknowledging this “really unique and surreal year called 2020” wherein we’re experiencing “a prolonged example of a disaster wrought by an invisible virus,” Collins introduced the event. “Covid-19 has profoundly affected all of us,” he said. “Nobody has gone through this without having a range of emotions, from stress, anxiety, fear—just grief about all the things that have happened and the lives that have been lost and the terrible stresses and economic distress that have happened to people…and certainly loneliness, the inability to gather together the way many of us love to do, which has not been possible with our requirements to be safely sheltered at home.”
The presentation was held on Sept. 10, World Suicide Prevention Day. Suicide is the nation’s 10th leading cause of death and is in many cases preventable.
“Concern in the U.S. about a rise in the suicide rate was already there before the pandemic, and now with covid, concern has grown,” Collins said. “Maybe we don’t entirely know the full impact of that yet, but certainly the sense of isolation, the loss of economic support [and] fear of illness cannot help with this circumstance of causing people who are already feeling the depression to take even more drastic action. We want to talk about these issues. We want to reinforce and support the fact that we at NIH care deeply about our staff and what you’re going through.”
Everly first gave what he called a “30,000-foot overview” of what is now his third pandemic as a consultant. He has advised policymakers and other national officials in Hong Kong with SARS, Singapore with H1N1 and now Covid-19, in addition to Ebola. He also has worked around the globe to address the mental health consequences of natural disasters, terrorist attacks and other catastrophes.
“[Covid] has been the most challenging,” he admitted.
“Anything that threatens mental health threatens the core of society,” Everly declared. “A nation will never recover from the effects of disaster until its people recover. Psychological recovery is not only important, but I would argue it’s the imperative.”
He said the coronavirus pandemic may give rise to a “hidden pandemic” that finds a high volume of folks in mental health crisis.
“People who previously coped well may ultimately succumb to the multiple stressors [that covid presents],” Everly explained. “People who were already suffering from a mental condition may get worse.”

Speaking directly to an NIH audience replete with pandemic scientists, physicians, nurses and other health care providers and affiliated employees, Everly cautioned that performance of such roles comes with tremendous costs—the most obvious and pernicious perhaps being burnout.
“Especially looking at frontline workers and first responders, we have seen heroic efforts on their parts, but not without a consequence—exhaustion being one,” Everly pointed out.
He explained why studying the psychology of an infectious disease is important and looked at issues specifically related to psychological impact of the pandemic.
Themes of distress that Everly’s team recorded among health care workers in Arizona include lack of clear information; new rules and responsibilities; overwhelming emotions such as worry and frustration; and conflicting emotions as well as concern for family members.
In a sample of more than 7,150 contacts compiled from late April to late August by the Mental, Emotional, Spiritual Health Collaborative at Johns Hopkins Medicine, Everly cited in excess of two dozen recurring commonalities. Among the more important to note are fear of infecting family members, physical fatigue, emotional exhaustion, feelings of isolation, fear of furlough or losing a job and distractions working from home or inability to stay focused on task.
“I want to reassure you that if you’re experiencing any of these, you’re not alone,” he said.
Everly also explored resilience and how some people seem better able to bounce back than others.
He and his team found several key characteristics that were common among firefighters, police officers, Navy SEALs and other military special ops team members as well as people who had recovered from catastrophic medical issues—active optimism, decisiveness, tenacity, following a moral compass and connectedness.
His group outlined several psychological phases of disasters, from impact to honeymoon through disillusionment until recovery/moving on. Using that timeline, Everly forecast a psychological trajectory and talked about estimating overall toxicity and casualty levels.
He closed his lecture with specific recommendations for fostering resiliency.
How do we help others bounce back? Everly cited 2003 Institute of Medicine research that suggested, “In the past decade, there has been a growing movement in the world to develop a concept similar to physical first aid for coping with stressful and traumatic events in life. This strategy…is most commonly referred to as ‘psychological first aid (PFA).’”
Not to be equated with mental health diagnosis or treatment, PFA provides a “compassionate and supportive presence designed to stabilize and mitigate acute distress, instill hope and facilitate access to continued mental health care,” Everly said.
Folks such as frontline workers who themselves are “facing a pandemic of exhaustion” could stave off its most harmful effects, Everly said, by adopting several strategies to recharge: exercise moderately every day, limit consumption of caffeine and other energy-boosting substances, get at least 7 hours of sleep per night, take a power nap when tired and practice some form of relaxation such as meditation, prayer, mindfulness or focused breathing.
Summing up, Everly shared several personal and family anecdotes about managing stress.
The presentation ended with an open conversation between Everly and Collins, who asked pointed questions about coping, including whether we should employ different coping tactics for short-term catastrophes as opposed to disasters, like this pandemic, that linger on.
“Different, definitely,” Everly replied. “The first thing is expectation. If we expect this to be short-lived, we have been remarkably, if not catastrophically, disappointed.”
He drew on lessons that World War II survivors recalled learning from the London Blitz, when what had at first been forecast as a massive but short-term air raid ultimately became a prolonged 9-month bombing campaign. Once they realized the onslaught was going to continue beyond early predictions, survivors’ mindsets began to recalibrate and their resolve formed.
The acceptance seemed to be a turning point for emotional recovery, Everly suggested. “The expectation, the self-fulfilling prophecy—the ‘What are we in for? We’re in for a long haul’—That in and of itself may be a game changer.”
The full session is archived at https://videocast.nih.gov/watch=38425.
