Small NIH Study Could Give Insight into Long-Term Neurological Symptoms of Covid-19
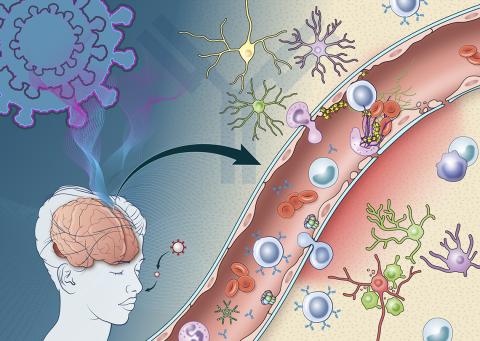
Photo: NIH Medical Arts
An NIH study describes the immune response triggered by Covid-19 infection that damages the brain’s blood vessels and may lead to short- and long-term neurological symptoms. In a study published in Brain, NINDS researchers examined brain changes in nine people who died suddenly after contracting SARS-CoV-2, the virus that causes Covid-19.
The scientists found evidence that antibodies—proteins produced by the immune system in response to viruses—are involved in an attack on the cells lining the brain’s blood vessels, leading to inflammation and damage. Consistent with an earlier study from the group, SARS-CoV-2 was not detected in the patients’ brains, suggesting the virus was not infecting the brain directly.
NINDS clinical director Dr. Avindra Nath and his team found that antibodies produced in response to Covid-19 may mistakenly target cells crucial to the blood-brain barrier. Tightly packed endothelial cells help form the blood-brain barrier. Damage to endothelial cells in blood vessels in the brain can lead to leakage of proteins from the blood, which causes bleeds and clots in some Covid-19 patients and can increase stroke risk.
For the first time, researchers observed deposits of immune complexes—molecules formed when antibodies bind antigens (foreign substances)—on the surface of endothelial cells in the brains of Covid-19 patients. Such immune complexes can damage tissue by triggering inflammation.
“Activation of the endothelial cells brings platelets that stick to the blood vessel walls, causing clots to form and leakage to occur,” Nath explained. “At the same time, the tight junctions between the endothelial cells get disrupted causing them to leak. Once leakage occurs, immune cells such as macrophages may come to repair the damage, setting up inflammation. This, in turn, causes damage to neurons.”
Researchers found that in areas with damage to endothelial cells, more than 300 genes showed decreased expression, while 6 genes were increased. These genes were associated with oxidative stress, DNA damage and metabolic dysregulation. This may provide clues to the molecular basis of neurological symptoms related to Covid-19.
Had the patients in the study survived, the researchers believe they would likely have developed long Covid. “It is quite possible that this same immune response persists in long Covid patients resulting in neuronal injury,” said Nath. “So these findings have very important therapeutic implications.”
