Probiotic Reduces Staph Colonization in Phase 2 Trial
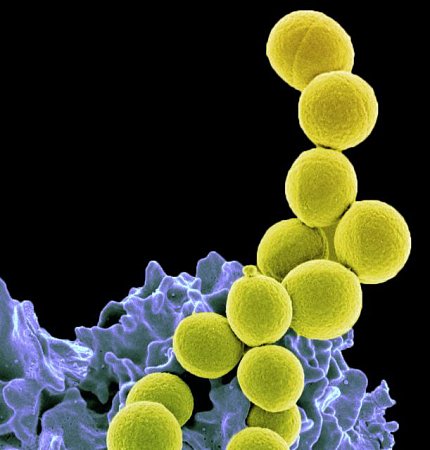
Photo: NIAID
A promising approach to control Staphylococcus aureus bacterial colonization in people—using a probiotic instead of antibiotics—was safe and highly effective in a phase 2 clinical trial.
The new study, reported in the Lancet Microbe, found that the probiotic Bacillus subtilis markedly reduced S. aureus colonization in trial participants without harming the gut microbiota, which includes beneficial bacteria. The research was conducted by an NIH team led by Dr. Michael Otto, a senior investigator at NIAID.
Methicillin-resistant S. aureus, or MRSA, is familiar to many as a cause of serious disease. Less well known is that S. aureus often lives in the nose, on the body and in the gut without causing harm. However, if the skin barrier is broken, or the immune system compromised, these colonizing bacteria can cause serious skin, bone, lung and blood infections.
Preventing S. aureus infections usings approaches that “decolonize” the body has gained increased attention as the spread of antibiotic resistance limits treatment options. Some decolonization strategies require large amounts of antibiotics, raising concerns about damaging the microbiota and perpetuating antibiotic resistance.
Probiotics—digestive supplements containing live microorganisms—may be a way to complement or replace antibiotics. Probiotic Bacillus is especially promising because it is administered orally as spores that can survive passage through the stomach and then temporarily grow in the intestine.
In the clinical trial, conducted in Thailand, the research team enrolled 115 healthy participants, all of whom were colonized naturally with S. aureus. A group of 55 people received B. subtilis probiotic once daily for four weeks; a control group of 60 people received a placebo. Researchers found no changes in the control group, but in the probiotic group they observed a 96.8% S. aureus reduction in the stool and a 65.4% reduction in the nose.
“The probiotic we use does not ‘kill’ S. aureus, but it specifically and strongly diminishes its capacity to colonize,” Otto said. “We think we can target the ‘bad’ S. aureus while leaving the composition of the microbiota intact.”
Researchers also found that levels of S. aureus bacteria in the gut far exceeded S. aureus in the nose, which for decades has been the focus of staph infection prevention research. This finding adds to the potential importance of S. aureus reduction in the gut.
The researchers noted their approach probably does not work as quickly as antibiotics, but can be used for long periods because the probiotic as used in the clinical trial does not cause harm.
