Jaffe Recounts Contributions to Lymphoma Research

The microscope is not an obsolete tool in the laboratory, said Dr. Elaine Jaffe, during a recent G. Burroughs Mider Lecture in the NIH Clinical Center’s Lipsett Amphitheater.
“Today, we have other tools to diagnose disease, but the microscope still plays an important role in disease discovery,” said Jaffe, NIH Distinguished Investigator in the National Cancer Institute’s (NCI) Laboratory of Pathology. There, she conducts pioneering studies related to the classification of malignant lymphomas.
More than a century ago, the German scientist Dr. Rudolf Virchow, now known as the “father of surgical pathology,” first described lymphoma under a microscope.
Microscopy has since played an important role in the clinical diagnosis and understanding of the pathogenesis of cancer, Jaffe said. Pathologists view tissue samples under a microscope and create a report with information about the cancer type, including the tumor grade, lymph node status, margin status and stage.
Lymphoma occurs when white blood cells called lymphocytes grow and form tumors in the lymph system, which is part of the body’s immune system. The lymph system is made up of tissues and organs that help protect the body from infection and disease. There are two types of lymphocytes: T cells and B cells.
More than 75 subtypes of the disease exist. Treatment depends on the type or subtype of lymphoma, and the distinction between Hodgkin lymphoma and “non-Hodgkin” lymphoma is less relevant today.
When Jaffe first started her career, pathologists had been using the Rappaport system of lymphoma classification, “a primitive approach” based on the size of a cell. It was developed before the discovery of T cells and B cells.
“When I first started at NCI as a resident in 1970, the stars were aligned for the revolution of lymphoma diagnosis,” she said.
Researchers at NIH were advancing the treatment of leukemia and lymphoma, gaining new insights in immunology and developing tools and techniques to characterize immune cells.
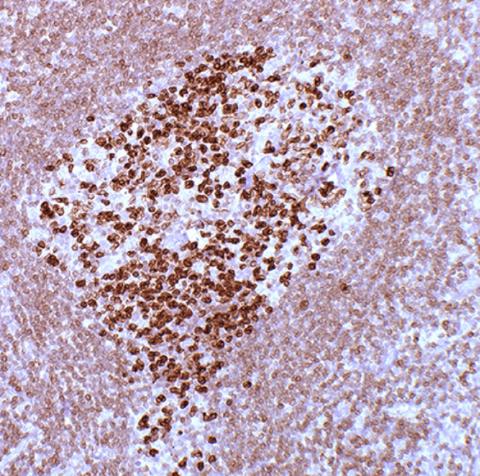
Photo: Dr. Elaine Jaffe
In 1974, Jaffe and her colleagues discovered that a common type of lymphoma—at the time called “nodular lymphoma”—originated in B cells and was derived from the lymphoid follicle, a key component of the B-cell immune system Their findings were published in the New England Journal of Medicine and that paper became a citation classic. This disease is now recognized as follicular lymphoma.
Her early research helped to replace descriptive classifications with those based on the latest findings in immunology and molecular biology. This approach also informed the development of today’s cancer therapies.
Over the next 20 years, technical advances enabled pathologists to study the nature of tumor cells in routine biopsy samples, helping to define the subtypes of lymphoma that looked different under the microscope as distinct disease entities.
In 1994, an international consortium of 19 pathologists developed the REAL classification, which “represented a new paradigm” in the classification of lymphoid neoplasms.
“Individual diseases were defined based on a constellation of clinical and laboratory features,” she said, including the appearance and structure of tumors, immunophenotype, genetic features and clinical presentation.
The REAL classification served as a model for defining all of the neoplasms derived from the hematopoietic system—lymphoid, myeloid and histiocytic tumors. It became the international standard for diagnosis on a worldwide basis.
“We fulfilled the ‘Holy Grail’ of lymphoma classification,” Jaffe explained. “We built a biomedical information network to promote disease discovery and pathogenic insights, provided a framework for precision medicine, facilitated clinical trials and improved the standard of diagnosis and treatment.”
Today, Jaffe and her colleagues continue to study lymphomas, both under the microscope, and with modern immunological and genomic tools. In one study, they discovered the earliest form of follicular lymphoma in biopsy tissue, termed “in situ follicular lymphoma.” The tumor cells have a translocation in the BCL2 gene, but do not have the subsequent hits that lead to clinically significant disease. This work provided insight into how these tumors arise and how they evolve over time.
Her laboratory also identified lineage plasticity in lymphoma. This was an unexpected discovery, in which B-cells can transform into histiocytes during the course of disease. Lineage plasticity can be a significant driver of cancer progression and drug resistance.
Finally, researchers in her lab observed overlap between Hodgkin and non-Hodgkin lymphomas, termed grey zone lymphoma, further indicating the plasticity of B-cells and the varied forms that evolve during lymphomagenesis.
The microscope is still a tool for disease discovery, Jaffe concluded. Many unique types and subtypes of lymphomas were first observed using the traditional light microscope employed in the daily care of patients. Such astute observations are often key to scientific discoveries regarding the origin and development of these diseases—taking us from the Bedside to the Bench.
The Mider Lecture was established in 1968 in honor of the first NIH director of laboratories and clinics and is presented annually by an NIH intramural scientist to recognize outstanding contributions to biomedical research.
