Inaugural Lecture
NIAID’s Marston Outlines Scientific Response to Coronavirus

While the Wednesday Afternoon Lecture Series goes on hiatus due to restrictions on travel and gathering imposed by the novel coronavirus, a new virtual lecture series has taken its place.
On Apr. 15, NIAID’s Dr. Hilary Marston became the first speaker in a series begun by the intramural program’s new COVID-19 scientific interest group (SIG), which began in March.
Her talk, “The Biomedical Research Response to COVID-19: A View from NIAID,” attracted nearly 1,200 viewers at the start and was introduced by Dr. Michael Gottesman, NIH deputy director for intramural research. He said the new SIG had already had more than 1,000 sign-ups to its listserv.
Marston, medical officer and policy advisor for global health and pandemic preparedness at NIAID, joined NIH in 2013 and has experience in outbreak response, including Zika virus and Ebola. She offered a broad overview of NIAID preparedness response.
“Part of NIAID’s mission is rapid response,” she said, “and the world has provided ample fodder [for pandemic preparation], for better or worse.”
NIAID leads the biomedical research response to emerging infectious diseases; in this role, it partners closely with other federal components, she explained. Other key players include three HHS entities—the Public Health Emergency Medical Countermeasures Enterprise, the Office of the Assistant Secretary for Preparedness and Response and the Biomedical Advanced Research and Development Authority—as well as the FDA, CDC, Department of Defense and other agencies.
Working in partnership with those agencies, scientific entities have taken one of three approaches to preparedness, she said.
- Priority-pathogen approach: “This is a list of all the scary viruses we know are out there, including Lassa, Ebola, MERS and SARS. It also includes Disease X, something that takes us all by surprise.”
- Vaccine platform technologies: Using a vaccine platform, such as a viral vector or nucleic acid material, researchers insert the gene or genes of interest from the pandemic threat.
- Prototype pathway: Here, researchers can leverage what they know about certain virus families, for example flaviviruses—which were deeply studied during the Zika outbreak of 2015-2017—to be ready for the next new or re-emerging disease. “We already had a significant amount of bench strength, and some ideas for a roadmap, from that experience,” Marston said.
The new coronavirus, SARS-CoV-2, “is quite large, about 30 kilodaltons,” said Marston. It belongs to a family of 4 viruses responsible for some 15-30 percent of common colds.
Coronaviruses were not thought to be associated with serious illness until SARS emerged in 2002 in Guangdong Province, China. Unlike COVID-19, which can have mild to virtually no effect on some of those infected, SARS had clear signs and symptoms.
“Most [infected] people had very clinically apparent illness,” said Marston. There were some 8,000 cases worldwide and nearly 800 deaths. “There was also a significant amount of economic disruption and a good deal of fear.”
SARS came under control within about a year due to basic public health measures, including containment and travel advisories, said Marston. The Vaccine Research Center (VRC) at NIH had a phase 1 SARS vaccine in trials within 20 months of full genome sequencing.
In 2012, Middle East respiratory syndrome, which is similar to SARS, emerged in Saudi Arabia in a camel host. Although it didn’t sicken the animals, MERS was nonetheless deadly in a few small outbreaks, including South Korea, where in 2015, 185 cases resulted in 33 deaths. Like SARS-CoV-2, MERS “tended to be severe in those with underlying medical problems,” said Marston.
As with SARS, countermeasure development for MERS quickly progressed in animal models, including mice and macaques.
“We knew that coronaviruses would be a constant epidemic threat,” said Marston. When COVID-19 broke out in China late in 2019, experts in the U.S. and abroad quickly suspected another coronavirus as the cause.
“Every country in the world is likely affected at this point,” said Marston.
Spread was exacerbated by factors including transportation. The virus was thought to have originated in a large seafood market in Wuhan, one of China’s largest cities.
“Now, however, we believe this was not the origin but a site of spread and outbreak amplification,” said Marston. The market is close to a high-speed rail line that connects Beijing and Hong Kong. “It was the perfect set-up for spread,” she noted.
The new coronavirus has a wide spectrum of effects, ranging from carriers who are asymptomatic to severe cases, including septic shock and multi-organ dysfunction.
“About 80 percent of cases are characterized as mild,” said Marston. Seventeen percent are severe and 2-3 percent are fatal. “There is a clear association with underlying disease and advanced age.”
For patients hospitalized with COVID-19, days 7 and 8 are crucial: “That’s when some patients take a turn for the worse, if it’s going to happen,” said Marston.
She reviewed the range of NIAID response, from basic research, through diagnostics (mostly conducted by CDC), therapeutics and vaccines. Some highlights:
- On Jan. 11, Chinese scientists published the SARS-CoV-2 genome in Science. “We were pleased it was shared so quickly,” said Marston. More than 200 genomes were posted globally within weeks, and the number continues to rise.
- NIAID scientists at the Rocky Mountain Laboratories quickly verified that the ACE-2 receptor in the lungs is the site of viral entry, “which is similar to SARS, but not to MERS,” Marston noted. RML scientists also discovered that several types of monkeys are a good disease model; other researchers are studying ferrets, guinea pigs, golden Syrian hamsters and mice.
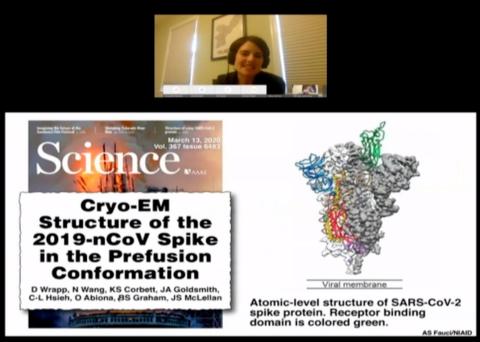
- VRC scientists Dr. Barney Graham and Dr. Kizzmekia Corbett characterized the structure of the virus’s pre-fusion spike and have an mRNA vaccine candidate in phase 1 trials. “We hope that this approach to antigen design might work across all of the coronaviruses,” Marston said, especially since there is a large animal reservoir of beta-coronaviruses, globally.
- A range of therapeutics have been identified that target the viral life cycle, including the virus itself and viral polymerase. The nucleoside analog remdesivir, used in Ebola and MERS (in animals), is being studied in a randomized controlled trial that began Feb. 25; results were expected in 4-6 weeks. The oral antiviral EIDD-2801 is being studied, as are hydroxychloroquine and azithromycin (in a French trial) and convalescent plasma (“NIAID is interested in hyperimmune globulin as a potential therapy,” said Marston).
In the future, Marston said her institute expects an expanded role in sero surveys, transmission and natural history of COVID-19, and perhaps the development of monoclonal antibodies.
During a Q&A session, Marston was asked if some current vaccines such as oral polio vaccine might offer cross-protection against COVID-19.
“That’s an interesting hypothesis,” she said, “and it’s gotten the attention of some great scientific minds.” There is some ecological data indicating that vaccines, including oral polio vaccine and especially BCG (used primarily against tuberculosis), are associated with lower rates of COVID-19, said Marston. “It may boost non-specific innate immunity in some way.”
Her full talk is available at https://videocast.nih.gov/watch=36375.
