Brain Study Tool
Harvard’s Brown Rethinks General Anesthesia

Harvard’s Dr. Emery Brown thinks general anesthesia should be considered a sub-discipline of neuroscience, not a sub-discipline of pharmacology, and he has the science—and art—to prove it.
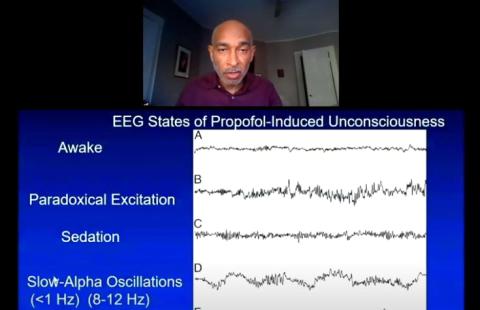
At a virtual version of the annual DeWitt Stetten Jr. Lecture, he focused mainly on propofol, which induces loss of consciousness, and how its administration—in micrograms per kilogram per minute—and effects can be tracked via electroencephalogram (EEG).
Brain waves tracked by EEG produce a colorful spectrogram, or video. It is a visual representation of the spectrum of frequencies of a signal as it changes over time. Brown likens it to abstract art: It can be both beautiful—especially in young patients ages 6-8, who tend to produce the most robust images—and scientifically informative.
He showed multiple videos that demonstrated graphically how oscillations in neural activity change as a patient proceeds from consciousness, to the sudden pinprick (and slight sting) of propofol—infused through a vein in the hand—to unconsciousness.
But it’s not enough that a patient is simply unconscious. After all, as Brown points out, “You need anesthesia because it hurts—surgery hurts.” Added goals of general anesthesia include analgesia or anti-nociception (pain relief), amnesia, akinesia (loss of movement) and physiological stability. And the patient has to wake up—preferably with a fairly clear head—when it’s all over.
“It’s not true that we don’t know how anesthesia works,” said Brown, who proceeded to demonstrate, via EEG videos, “the rich temporal and spatial dynamic” as propofol, in a classic pattern—especially in patients ages 18-35—induces brain stem inactivation in patients. “We can see a large number of circuits in the brain, all doing the same thing.”
The most common pattern, he has written in past journal articles, is a progressive increase in low-frequency, high-amplitude activity as the level of general anesthesia deepens.
Anesthesia provides “the strongest use of an EEG signal,” he said. “It also provides the most information about the brain state, but most anesthesiologists don’t use it.”
Only about a quarter of the field employs the technique, “and those using it aren’t using it the way we are here,” said Brown, who is the Warren M. Zapol professor of anaesthesia at Harvard Medical School and Massachusetts General Hospital (MGH), the Edward Hood Taplin professor of medical engineering and of computational neuroscience at Massachusetts Institute of Technology and a practicing MGH anesthesiologist.
His team is gaining insights into the cortical dynamics of the anesthetized state by studying patients with epilepsy who have implants that allow recording of neuron spiking, and the measure of field potentials. Why care about how propofol affects spike rates in this population? “So we can understand what happens in the human brain under anesthesia, because [patients’] awareness should never happen now during surgery,” said Brown.
Different anesthetics have different EEG signatures, he explained. “It has to do with where the receptors are that they target, and subsequent circuit dynamics they induce.”
And the brain’s response to anesthesia changes dramatically with age.
“There are much weaker oscillations with advanced age,” Brown said. “Circuits start to break down, myelin breaks down, mitochondria, too…We get a diminished signal. How well we take care of ourselves is also important.”
Kids, he disclosed, “have really gorgeous spectrograms—almost like abstract art.”
Brown and his colleagues are now taking a multi-modal approach to general anesthesia, employing up to 10 drugs—including a multi-drug regimen for anti-nociception--for a procedure as routine as appendectomy.
“We can wake people up on a dime, and with a much clearer head, if well-managed,” he said. “We have better control of both nociception and unconsciousness.”
Another population Brown has found it advantageous to study are patients in a medically induced coma, which can be used therapeutically to treat refractory epileptic seizures, or to reduce intracranial pressure in people with a brain injury.
“Burst suppression, a profound state of anesthesia, is the target for these patients,” he explained. Because the patient often needs to be maintained in this state for several days, it is a perfect opportunity to develop a computer-guided control system that monitors the EEG and controls the infusion of propofol on a second-to-second basis to maintain a therapeutic state of burst suppression. “Precise control of the brain state is our goal.”
Use of multiple different anesthetics to control nociception is “an obvious way to move away from the use of opioids…Furthermore, we can learn a lot about the brain by studying anesthesia,” Brown concluded.
During a brief Q&A, Brown was able to make a few more points:
- A patient’s history of drug use affects dramatically an anesthesiologist’s decision-making. “It takes very little to anesthetize an acutely intoxicated patient,” said Brown. Those with compromised livers may have prolonged effect of anesthesia. Cocaine use is important to know, as is marijuana use. “We’re trying to sort that [marijuana] out now—there’s not a clear picture of it. We’re going to sort that out in the next few years.”
- While treating a rugby player in his 30s, Brown noted that he had the EEG of a 70-year-old. Brown called it a “tantalizing possibility” to use EEG diagnostically to determine a patient’s brain age.
- Brown no longer uses anesthetic gases—a variety of ethers—because they are both pollutants and are not as effective as propofol. “I stopped using gases 4 years ago,” he said. “I can titrate much more effectively with propofol.”
The full talk is available at https://videocast.nih.gov/watch=40044.
