Doudna Describes Exciting Future for CRISPR

Photo: Chia-Chi Charlie Chang
CRISPR genome editing is a powerful tool that can treat many genetic diseases. If it’s to reach its full potential, scientists must develop new delivery methods, said CRISPR pioneer Dr. Jennifer Doudna during an NIH Director’s Lecture in Masur Auditorium.
“Even if we have a great genome editor, we still have to get it into cells,” said Doudna, Nobel laureate in chemistry (2020) and professor of biochemistry, biophysics and structural biology at the University of California, Berkeley.
Often described as “genetic scissors,” CRISPR is a revolutionary tool that allows scientists to selectively modify the DNA of living organisms. Short for clustered regularly interspaced short palindromic repeats, CRISPR is a defense system that bacteria use to prevent infection. CRISPR technology is based on this system and can be engineered to make targeted changes to a genome.
Doudna started out in the field by trying to answer a “fundamental question in biology, namely, how bacteria fight viral infections.” She became interested after a colleague at Berkeley, Jill Banfield, theorized that bacteria have an adaptive immune system that uses RNA molecules to protect cells from future infection.
In 2012, Doudna and French scientist Dr. Emmanuelle Charpentier published their seminal paper on Cas9, an enzyme that uses an RNA guide in bacteria to bind to and then cut strands of DNA. Since then, scientists have identified large families of these enzymes in bacteria. They protect bacteria from infection or plasmid transformation.
“Amazingly, they can also be harnessed as technologies for manipulating genomes,” Doudna said. “That’s something we’ve been working on for over 10 years.”
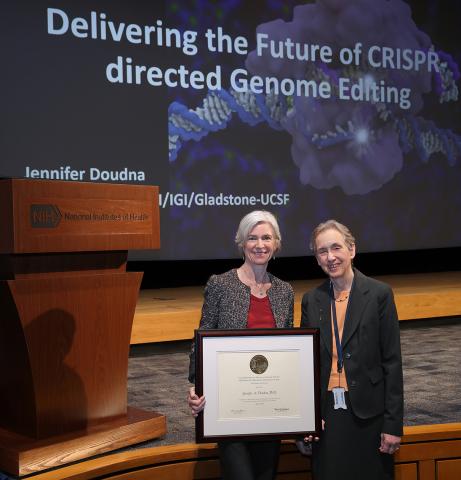
Photo: Chia-Chi Charlie Chang
Last December, the FDA approved the first CRISPR therapy to treat sickle cell disease, a group of inherited red blood cell disorders that affect hemoglobin, the protein that carries oxygen through the body.
“What’s extraordinary about this type of therapy is it’s a one-and-done treatment that can correct a disease-causing mutation—or in the case of sickle cell disease—override the effect of a genetic mutation. This is incredibly motivating,” she said. “Yet, we’re still at the very beginning of this field and what will be possible with CRISPR.”
The treatment uses the same CRISPR enzyme Doudna and Charpentier studied more than a decade ago, Cas9.
Although there are many more enzymes out there now, Doudna said Cas9 is “still one of the very best for manipulating genomes for reasons that we’re still working to understand.”
While CRISPR-based therapies are very exciting, “we have to grapple with the challenges, including the cost and the difficulty of delivering CRISPR into patients,” she explained. Right now, a doctor removes a patient’s bone marrow stem cells and edits the cells in a lab. The edited cells are returned after the patient’s bone marrow is destroyed.
“We imagine a day where that won’t be necessary,” she said. “It could be possible to deliver the CRISPR genome editor directly into patients.”
Doudna and her colleagues are now focused on improving Cas9 gene editors, even though they are already effective enough to use clinically.
Having enzymes that are robust, stable and very active at low concentrations “will be critical for reducing the amount of enzymes that you need to use in the clinic and for improving the specificity and the kinds of editing efficiencies that we can observe over time,” she pointed out.
In 2017, her lab at the Innovative Genomics Institute started studying a protein from a thermophilic bacteria, or microbes that live in high-temperature environments, such as hot springs or deep-sea hydrothermal vents. Called GeoCas9, the high-temp protein has a similar structure—“a classic, clam shell shape that holds onto the RNA guide”—to other Cas9 proteins.
“These proteins work by using their RNA guides to interrogate DNA in a genome and identify sequences that match the RNA guide,” she explained.
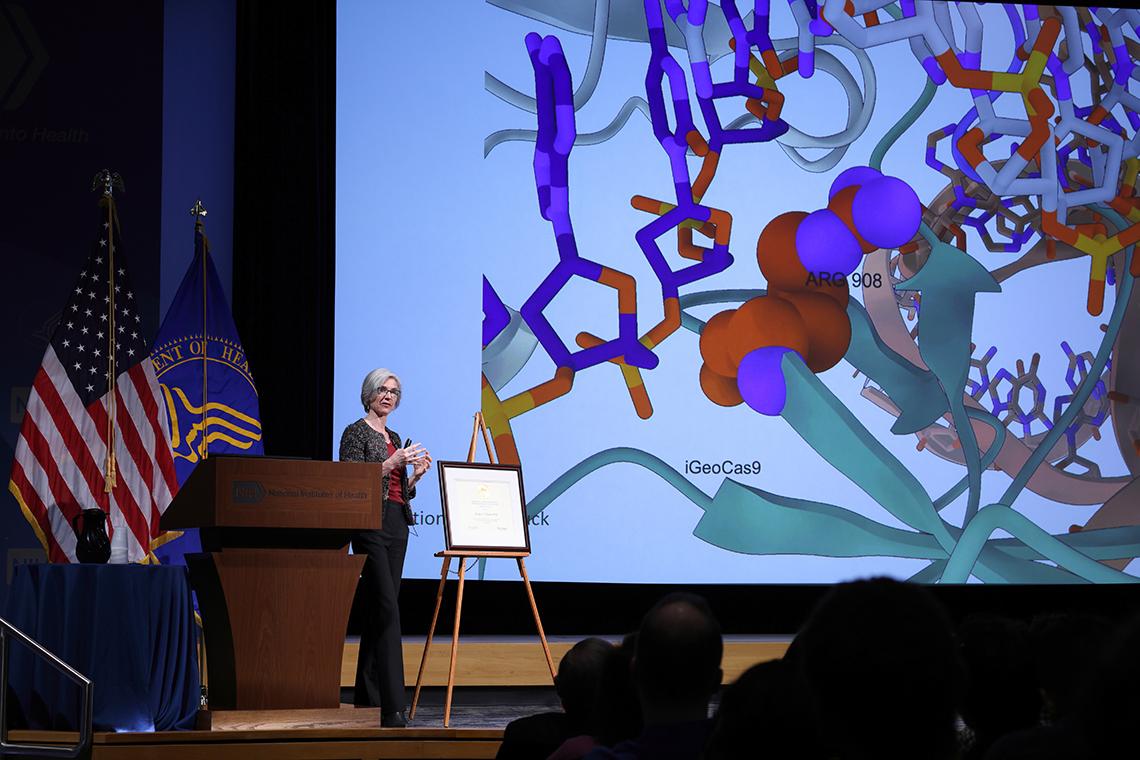
Photo: Chia-Chi Charlie Chang
Compared to Cas9, GeoCas9 remains active at much higher temperatures. Perhaps because of this thermostability, GeoCas9 is highly stable in the presence of human serum, she said. Research is ongoing.
According to Doudna, figuring out how to deliver these treatments in vivo is at the “forefront of the field.” Most patients who can benefit from an approved therapy using CRISPR-Cas9 can’t access it because of the cost or the lengthy hospital stay as a result of a bone marrow transplant.
“What if we have a mechanism for delivery that would allow us to put these editing enzymes safely and efficiently into just the cells of the body where they could have clinical benefit?” she remarked. “It would be transformative.”
Doudna’s lab is studying several techniques to deliver CRISPR treatments more efficiently. Research “points in a direction that’s very promising.” A few years ago, a postdoctoral student, Jenny Hamilton, demonstrated that the exterior envelope of a virus could be emptied and filled with Cas9 for precise gene editing in vivo.
Since then, these enveloped viruses have been altered so much that they are now referred to as enveloped delivery vehicles (EDVs). These EDVs are wrapped up like a virus and have molecular machinery on the surface that can recognize target cells. However, they are not infectious and they don’t carry a viral genome.
“We’ve been working on how these EDVs are put together and how we can make them better,” she said.
Improving the accuracy and delivery of CRISPR therapies to reduce the cost will make these treatments “that can be much more widely available ultimately globally,” Doudna concluded.


