Investigator Studies How the Environment Affects Asthma
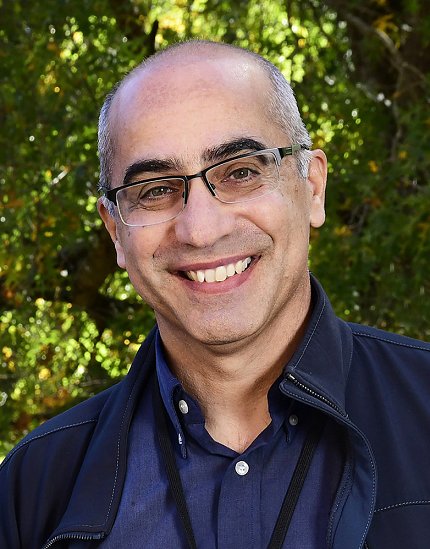
Photo: Steve McCaw/NIEHS
Asthma affects about 25 million people in the United States, including 4.7 million children and adolescents. Environmental exposures can worsen the coughing, wheezing, chest tightness and shortness of breath symptoms linked with asthma.
NIH research highlights the importance of taking each patient’s unique environmental exposures into account when treating asthma. The lung disease occurs when the body’s natural defenses against germs and sickness react strongly to environmental exposures like pollen or pollutants.
Dr. Stavros Garantziotis, a lung doctor and head of the Matrix Biology Research Group at NIH’s National Institute of Environmental Health Sciences (NIEHS), recently discussed specific exposures driving asthma and how people’s immune systems react differently.
“Personalized environmental medicine—which means evaluating each person’s specific exposures and susceptibility factors and tailoring treatment specifically to their needs—I believe can help prevent or even reverse some lung diseases,” said Garantziotis.
Where people live, work and play can affect asthma symptoms and severity. “Looking only for asthma symptoms and ignoring the exposures that may have caused these symptoms provides an incomplete picture,” he noted. “It is like photoshopping the patient out of a photo; you lose a huge amount of information.”
NIEHS research has started to move the needle so that doctors are more aware of the role of environmental exposures in asthma.
“Personally, I have been able to improve symptoms and even reduce the amount of medication my asthma patients need by thoroughly evaluating their exposure profiles and taking steps to address them. These are low-cost, low-tech, but high-impact solutions that can help patients tremendously.”
Garantziotis has been studying a protein called TLR5, which he believes plays a central role in lung disease because it helps regulate immune responses to environmental injury.
For example, his team found that house dust in many homes of asthma patients activates TLR5 leading to an overactive immune response. This is probably caused by house dust bacteria shedding proteins that activate TLR5. Often, these bacteria are found in the excrement of house pests like cockroaches or mice. Cleaning up these sources of TLR5 activation is a simple and effective non-medication way to prevent asthma flare-ups caused by this pathway.
Garantziotis also shared advice he gives to empower his patients.
“I always talk to my patients about their home and work environments,” he said. “I ask them to become detectives in their own asthma cases. Often, they start recognizing patterns of exposure and symptom associations. [Some] might feel sicker at home compared to when they are away or have more symptoms in the morning or at night. Such information helps them better manage their symptoms.”
It’s critical that patients learn how to manage their symptoms and take control of their asthma, he said. “After all, they visit my clinic only once every six months, but they are experiencing asthma 24/7.” —adapted from NIEHS’s Environmental Factor
For more information about NIH’s asthma research, explore these resources:
