Model Predictions
Viboud’s Covid Transmission Data Guides Policy

Getting through and beyond an infectious disease pandemic takes a lot of planning. To determine which interventions might have the greatest impact, decision-makers continually rely on data projections. Based on these models, they consider degrees of reopening, vaccination priorities and other strategies to help control transmission, prevent deaths and move toward normalcy.
One of these disease modelers who’s busy plugging in the stats and plotting out possible trajectories is Dr. Cécile Viboud, senior staff scientist in FIC’s Division of International Epidemiology and Population Studies. She spoke virtually to NIH’s Covid-19 interest group recently about the virus’s transmission and mortality dynamics.
In forecasting trends, there’s a lot to learn from other disease outbreaks such as dengue, Ebola and flu, the latter of which is Viboud’s focus in non-pandemic times.
“If we’re able to predict transmission rates 3 to 4 weeks ahead, this has some value in terms of situational awareness,” she said. But long-term projections are more complicated.
“We have a similar disconnect between weather and climate in the disease world,” she explained. “In the same way that weather produces a short-term forecast, we in infectious diseases also are able to relatively accurately predict what’s going to happen in the next few weeks. If we think of more long-term projections—similar to climate—it’s much more difficult, of course. In the longer term, a lot of things can change,” from population behavior to interventions.
There will always be uncertainties that create some outliers during a pandemic, which is why Viboud and fellow epidemiologists turned to ensemble projections from multiple models.
Impact of Interventions

In spring 2020, Viboud and colleagues set out to project the Covid outbreak over 6 months in a small, rural U.S. county to guide its reopening strategy. Her group helped coordinate projections from 17 academic teams who were tasked with modeling infections, hospitalizations and deaths and the probability of a new outbreak from May to November based on different interventions—from stay-at-home orders to reopening workplaces at different intervals.
Some clear, obvious results came from every model: health outcomes would improve by remaining closed; relaxing restrictions too soon would cause a surge in cases and hospitalizations.
Interestingly, when comparing ensemble projections across the models with what actually happened in 66 U.S. counties of similar size that remained closed through Aug. 31, Viboud said, “the model data really aligns well at the 6-month timescale with observations.”
Vaccine Scenarios
The project was extended to look at the next 6 months, based on 4 vaccine scenarios designed by the CDC and then President-elect Joe Biden’s transition team. A collaboration among NIH and Penn State and Johns Hopkins universities, first-round projections were released on Jan. 6.
The scenarios were:
- Optimistic—a fast rollout of 25 million doses per month of highly effective vaccines, with nonpharmaceutical interventions (NPI)—such as distancing, testing, contact tracing—remaining high for 6 weeks then slowly tapering off
- Moderate—a slower vaccine rollout of lower efficacy vaccines with a faster decline in NPI starting at 3 weeks
- Fatigue—a slower vaccine rollout of high-efficacy vaccines but, due to hesitancy, only half the population accepts it
- Counterfactual—no vaccine along with a fast NPI decline
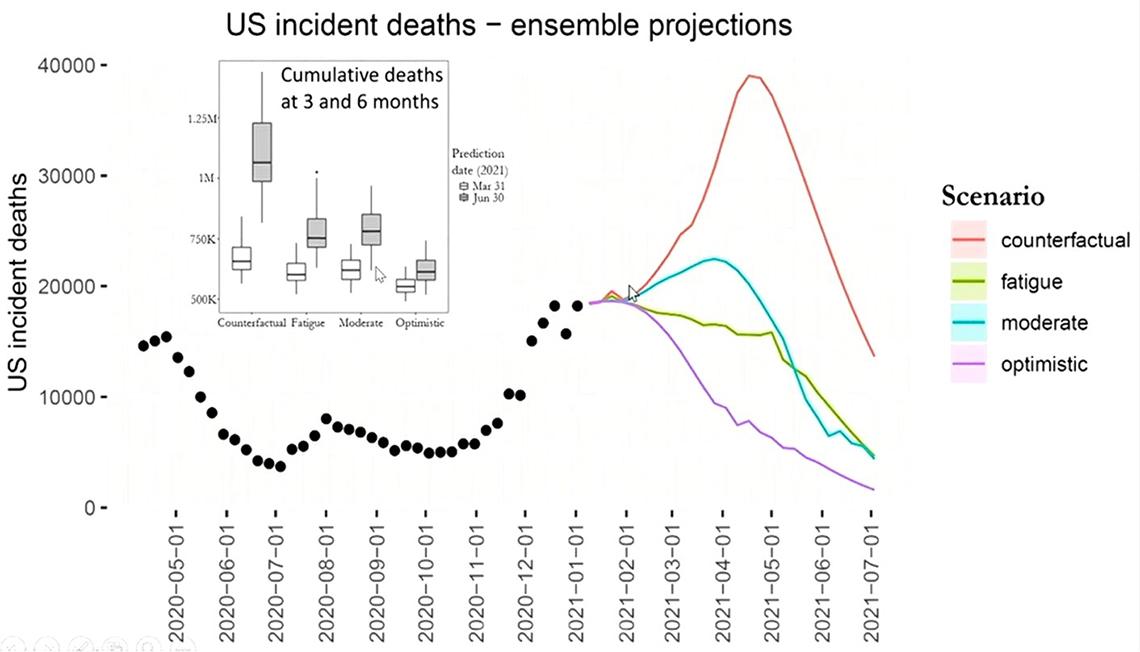
As expected, the models all show a modest, steady case decline in the optimistic scenario, while the other three predict a resurgence in cases before declining. All six models show the U.S. in a better place by July 1, with hospitalizations and deaths decreasing. The question is how bad it gets before it gets better.
“In vaccine scenarios, we see a faster decrease in hospitalizations and deaths than we see in cases and that’s because of the vaccination scheme that’s targeting high-risk groups before the general population,” said Viboud.
The optimistic, best-case scenario predicts upwards of 600,000 U.S. deaths by June 2021. But the most realistic trajectory back in January was a combination of the moderate and fatigue scenarios. Currently, models are getting tweaked to evaluate new-variant scenarios—a more-contagious U.K. variant and a South African one that seems to evade natural immunity.
Mortality Patterns
One way to quantify the burden of infection during a pandemic is to look at excess mortality: that is, taking mortality data from previous years, in normal times, and attributing deaths exceeding that baseline to the pandemic.
The most specific indicator of Covid’s impact is excess respiratory deaths, which have matched closely with official Covid-19 mortality statistics. There’s also a high correlation between excess burden of Covid and high rates of certain diseases.
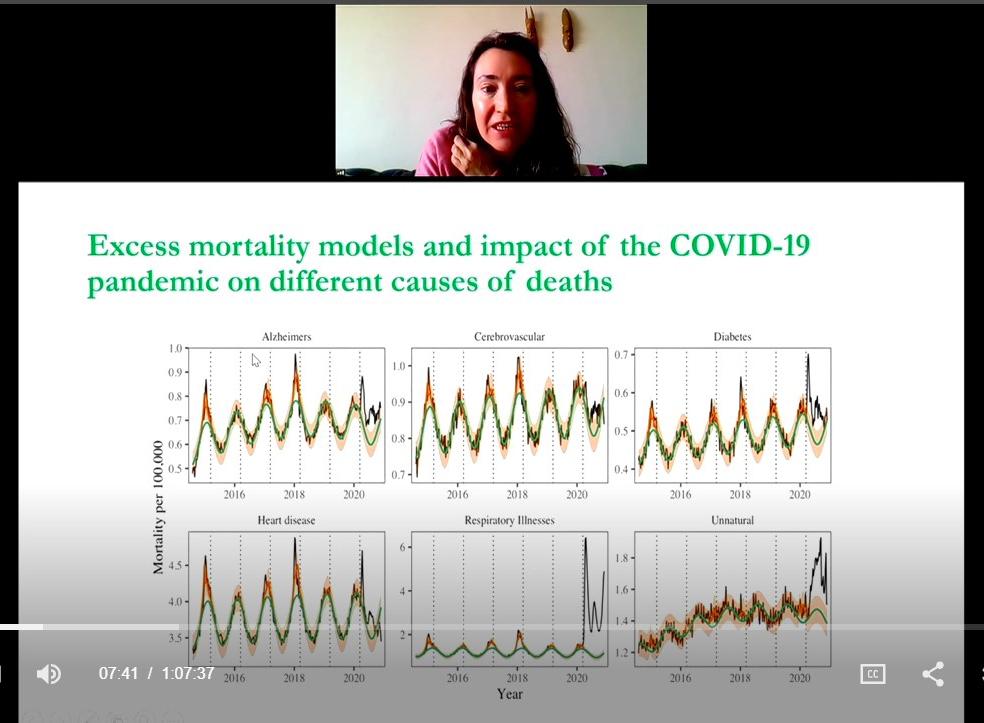
“This suggests that maybe Covid has a direct impact on diabetes, heart disease and cerebrovascular disease,” Viboud said.
In the U.S., 82 percent of all-cause excess deaths are confirmed as Covid-19 fatalities, a rate that’s been stable since summer 2020, she said. Of the remaining 18 percent, at least 8 percent are indirect increases in unnatural causes, such as injuries, suicides or drug overdoses, and secondary impacts that did not follow the Covid trajectory.
“What’s quite striking is the number of excess deaths in young individuals [ages 25-44] that’s not directly attributed to Covid-19,” she said.
Overall, compared with flu pandemics, as of Nov. 30, the excess Covid death rate was 6 times that of a severe flu season and 24 times greater than the 2009 flu pandemic.
Going Global
Also critical to Viboud’s research is looking at global data and the outcomes of pandemic-related policy decisions in other countries.
With contacts in China, her team is looking at the impact of social distancing in Shanghai and whether tracking population mobility through digital contact tracing sufficiently interrupted viral transmission without the burdens of lockdown.
Viboud’s long-term collaboration on influenza with South Africa’s National Institutes of Communicable Diseases has extended to studying Covid hospitalization trends. A small serology survey last summer in Capetown found a high Covid attack rate across all age groups that captured infection up to the first peak. Viboud’s South African colleagues thought they were out of the woods, but the country experienced a second wave, spurred by the new Covid variant.
“If you want to quantify the burden of a pandemic, you have to quantify the total—all of the positive and negative impacts,” Viboud emphasized.
Among the positives are the pandemic health measures, from hygiene to masking, that have decreased the circulation of other pathogens. It’s a major reason why, for example, in South Africa last year, hospitals saw far fewer children with respiratory illnesses than in previous years.
Among negative impacts are the effects of averting the health care system and therefore not getting tested and treated for new and existing conditions.
“One question,” said Viboud, “is whether those illnesses are going to be unattended and show up as deaths later on.”
