Highly Unlikely, but Possible
Pandori Discusses What We Know About Covid Re-Infections
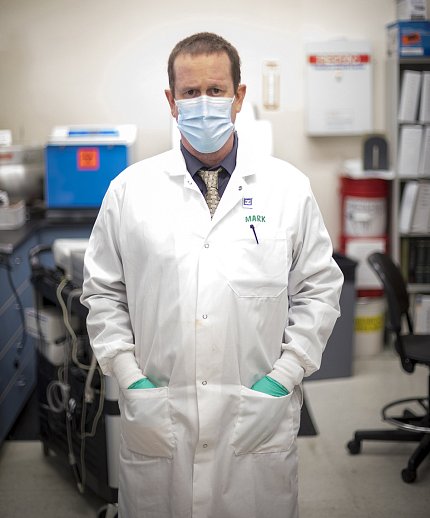
Individuals who have recovered from SARS-CoV-2 may still be at risk for re-infection, said Dr. Mark Pandori, director of the Nevada State Public Health Laboratory (NSPHL) and associate professor of pathology at the University of Nevada, Reno School of Medicine. He spoke at a recent Covid-19 Insights Seminar hosted by NHLBI.
In his lecture, “Re-infection with SARS-CoV-2 and its Impact on Covid-19 and Public Health,” Pandori discussed his efforts with NSPHL to identify re-infections and what these cases mean for the future of the pandemic.
His first experience with Covid-19 re-infection came in the beginning of the coronavirus crisis. A young man tested positive and was symptomatic for a month. He then had 2 consecutive negative tests and was symptom-free for 48 days before developing symptoms again and testing positive. The new round of Covid was more severe. The individual was hospitalized for low blood oxygen levels, but recovered quickly.
How could Pandori confirm that it was truly a re-infection? The patient lived with his mother, who also developed Covid at the same time as her son’s second illness, which increased the likelihood that the man’s infections were two distinct events. Pandori still needed a concrete method to validate his theory, so he decided to sequence the viral genomes from the man’s positive tests.
“Covid mutates at a rate of about 2 base pairs per month,” Pandori said, “so, if it had remained dormant in the individual for the 48 days between the 2 cases, then we would expect it to have mutated enough to change about 3 base pairs.”
Base pairs are the subunits of genetic material: DNA in us, and RNA in viruses such as Covid-19. Mutations are often the result of changes in base pairs. Those changes may do nothing at all or may change a gene enough to alter its function. If a mutation creates a change that is helpful to the organism, such as making a virus more infectious, that mutated strain will become more common in the population.
Pandori sequenced the genomes from the two different infections (cases A and B) and found that there was “considerable genetic distance” between them. There were 11 differences in base pairs between cases A and B—far more than the 2 or 3 that would be expected if this was the same illness that had lain dormant in the body between the 2 periods of symptomatic infection.
Other researchers throughout the world have been sequencing the genomes of Covid-19 infections and have constructed a map of all the different strains and their relatedness.
Case A looked like the strain that was circulating in Nevada at the time, while case B resembled the version of the virus that had initially emerged from Wuhan—the ancestral genotype. The odds of the virus from case A changing that drastically and reverting closer to the ancestral genotype were “vanishingly small,” therefore making re-infection the most likely explanation.
Other instances of re-infection began to emerge around the same time as Pandori’s first subject (in Nevada and around the world), and he was able to confirm several other cases through genomic sequencing.
Re-infection is still highly unlikely in most cases, Pandori said, but he is concerned that the virus will evolve the ability to mutate faster and possibly make vaccines less efficacious.
NIH’ers can view the entire lecture at https://videocast.nih.gov/watch=40179.
