Designing a Safer Antifungal Drug
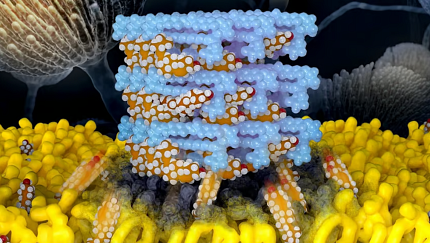
Photo: JOSE VAZQUEZ/UNIVERSITY OF ILLINOIS
Every year, more than 1.5 million people worldwide die of a fungal infection. Fungi tend not to harm healthy people, but individuals with a suppressed immune system are vulnerable to serious fungal infections.
Some currently available antifungal drugs are becoming less effective as fungi develop resistance to them. Many of the remaining drugs are highly toxic.
One of these drugs, amphotericin B (AmB), is based on a natural product produced by bacteria. AmB may be given as a last option when other antifungal drugs have failed. But it damages cells in the kidneys, limiting the dose that can be used.
For several years, a research team led by Dr. Martin Burke at the University of Illinois Urbana-Champaign has been studying AmB toward finding a way to reduce its toxicity. Burke and his team discovered that AmB works by drawing a fungal molecule similar to cholesterol, called ergosterol, out of the membranes, which results in cellular damage and death. The team discovered that AmB does the same thing to cholesterol in human cells, causing the damage observed in kidneys.
In a new study, funded in part by NIH, scientists altered AmB to better grab ergosterol while leaving cholesterol intact. Results were published in Nature.
The new compound was virtually nontoxic when tested in cells and mice, but it was less potent than AmB because it removed ergosterol from fungal cell membranes less rapidly. This gave the fungal cells time to produce enough extra ergosterol to survive.
To improve efficacy, the researchers made another tweak to the structure. The resulting compound, called AM-2-19, drew ergosterol from fungal cells rapidly but left cholesterol unaffected.
AM-2-19 proved to be safe when given in high doses to human cells and mice. Crucially, it was also as or more effective than AmB against more than 500 strains of pathogenic fungi. When tested against several potentially deadly fungal pathogens in mice, including members of the Candida, Aspergillus, and Rhizopus families, AM-2-19 eradicated several strains entirely at high doses.
AM-2-19 has been licensed to Sfunga Therapeutics and recently entered a phase 1 clinical trial.—Sharon Reynolds, adapted from NIH Research Matters
