NIDCR Celebrates Its History, Looks Ahead
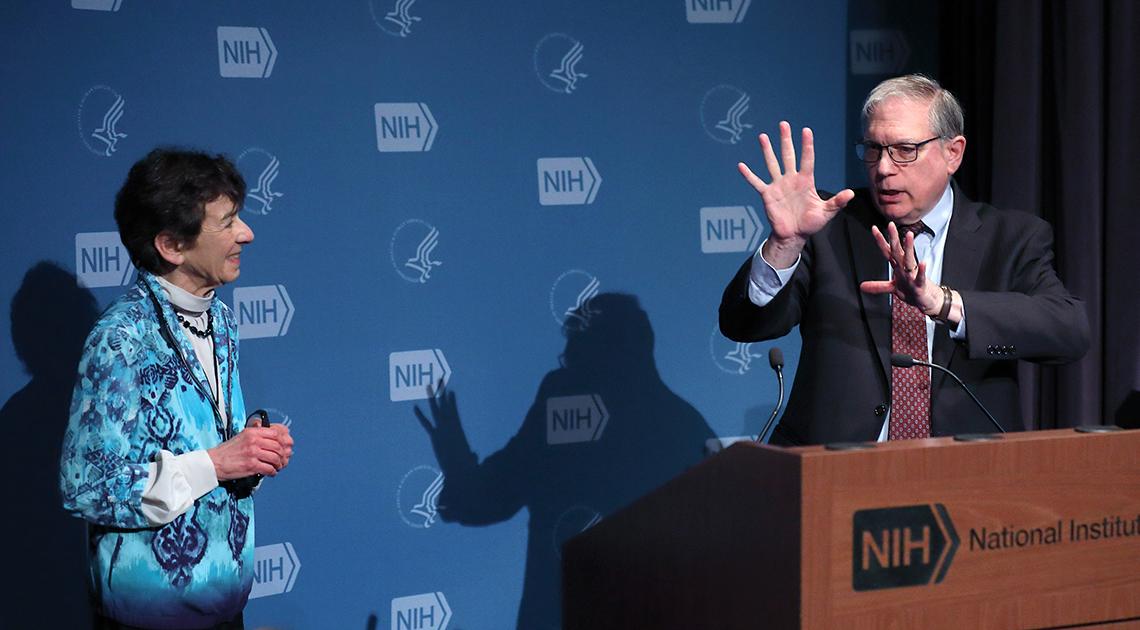
Photo: Chia-Chi Charlie Chang
NIDCR celebrated its origins and set its course toward 2030 during a recent craniofacial research symposium to mark its 70th year. “We were one of the first institutes,” said Dr. Martha Somerman, NIDCR director. She described the “incredible epidemic of infectious disease of the oral cavity”—commonly known as tooth decay—that had disqualified men and women from military service in World War II as the impetus to form a dental research institute.
“Looking Back and Facing the Future: From NIDR to NIDCR,” held in Lipsett Amphitheater on May 6, highlighted how science and clinical care have changed since 1948, when NIDCR’s predecessor, the National Institute of Dental Research, was created by Congress. The symposium’s speakers, a mix of NIDCR intramural and extramural scientists, covered craniofacial anomalies, tissue regeneration, skeletal development, wound healing, periodontal disease, salivary biology and other topics.
To more accurately reflect the institute’s scope of research, “Craniofacial” was added to NIDR’s name in 1998 during the tenure of Dr. Harold Slavkin, NIDCR’s director from 1995 to 2000. He recounted some of the earliest work in the field by a Pennsylvania orthodontist named Dr. Herbert Cooper.
In Lancaster County, where he practiced, Cooper noticed many individuals with craniofacial deformities. “He felt overwhelmed,” said Slavkin, so Cooper enlisted the help of the community’s social services providers, pharmacists, pediatricians and speech and language professionals. With these people, he created care teams, and, in 1938, Cooper formed the Lancaster Cleft Palate Clinic.
Today, interprofessional health care teams are used around the world to help people with both congenital and acquired craniofacial anomalies. The impact of these disorders is great, said Slavkin, dean emeritus of the Herman Ostrow School of Dentistry, University of Southern California. He said in the United States, a million people have serious craniofacial defects. He estimated that the total direct and indirect global health care costs for these conditions are around $500 billion per year.
“Our face is our identity,” said Dr. Yang Chai, a professor, surgeon and director of USC’s Center for Craniofacial Molecular Biology. When there are defects, it affects quality of life.
To improve outcomes for people with cleft palate, a common birth defect, Chai’s lab explores several research threads. Data from FaceBase, an NIDCR-funded resource for craniofacial researchers, helped Chai and his colleagues create a mouse model that has let them understand soft palate development. Critical for swallowing, breathing and speaking, the soft palate is often affected in patients with cleft palate.
His lab also has teamed up with biomedical engineers to make a 3-D printed scaffold that can be seeded with stem cells and placed into defective bone to prompt its regeneration. In animal studies, this method has led to high-quality bone regeneration, said Chai. His goal is to use 3-D scaffolds to better repair cleft palates and other craniofacial defects in humans.

Photo: Chia-Chi Charlie Chang
Like Chai, Dr. Chia Soo aims to improve the body’s ability to heal. She and her colleagues at UCLA’s School of Medicine have shown that a protein called fibromodulin is required for scarless tissue repair in rodents. Soo’s group has spent the two decades since that discovery developing a fibromodulin-based peptide therapy that is currently being tested in clinical trials for its safety and efficacy for human wounds. If successful, the compound may be used to reduce scarring during surgery.
Her team found that the periodontal lesions of people with LAD1 have an overabundance of immune cells called T helper 17 (Th17) cells. The researchers have tested a drug called ustekinumab that targets Th17 cells.
One 19-year-old patient with LAD1 had such severe periodontal disease that he had begun losing the bone supporting his teeth; Moutsopoulos wanted to find a way to save them. After receiving the drug, the young man’s oral condition improved, as did an open lesion on his back. These findings are leading to insights into the mechanisms and potential treatments for the more common form of periodontal disease that affects up to half of U.S. adults.
Going forward, what do NIDCR’s former and current directors hope for? For Dr. Lawrence Tabak, NIH principal deputy director and NIDCR’s director from 2000 to 2010, it is to take full advantage of the power of data. “Our ability to collect and analyze data at scales that 8 to 10 years ago we could not have imagined is today a real possibility,” he said.
Slavkin wishes to see more “evidence-based policy making,” and the possibility that “all people have comprehensive, quality health care.”
Dental, oral and craniofacial research is moving forward on many fronts, said Somerman, who outlined research priorities that emerged from the institute’s strategic visioning initiative, NIDCR 2030.
She envisions a future where patients benefit from autotherapies that harness the body’s ability to heal itself. She looks forward to the availability of more comprehensive salivary diagnostics, improvements in machine learning to speed diagnosis, increased understanding of the microbes that reside in us and more public-private partnerships to get treatments to patients faster.
By 2030, Somerman said, dental, oral and craniofacial health should “be understood within the context of the whole body,” and precision health should be available for everyone.
